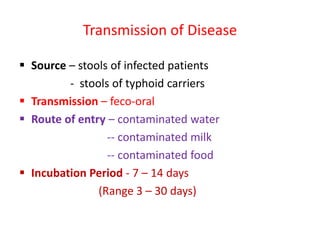
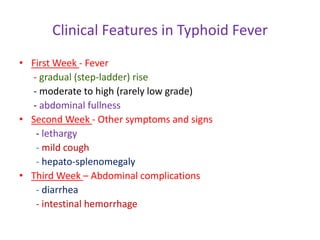
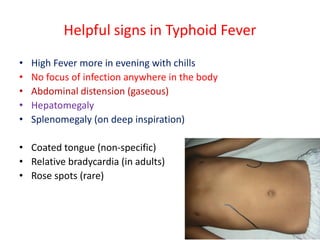
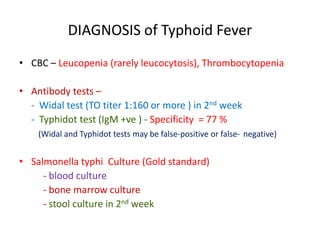
An 8-year-old child presents with a fever of 104°F for the past 8 days. On examination, the child has mild diarrhea, abdominal distension, hepatomegaly, and splenomegaly. The likely clinical diagnosis is typhoid fever, an infectious disease caused by Salmonella enterica serovar Typhi characterized by high fever and abdominal symptoms. Typhoid fever is transmitted through contaminated food or water and has an incubation period of 7-14 days. Common clinical features include a gradual rise in fever, abdominal symptoms, and hepatosplenomegaly. Complications can include intestinal hemorrhage or perforation. Diagnosis is confirmed through blood culture but antibody tests and culture of