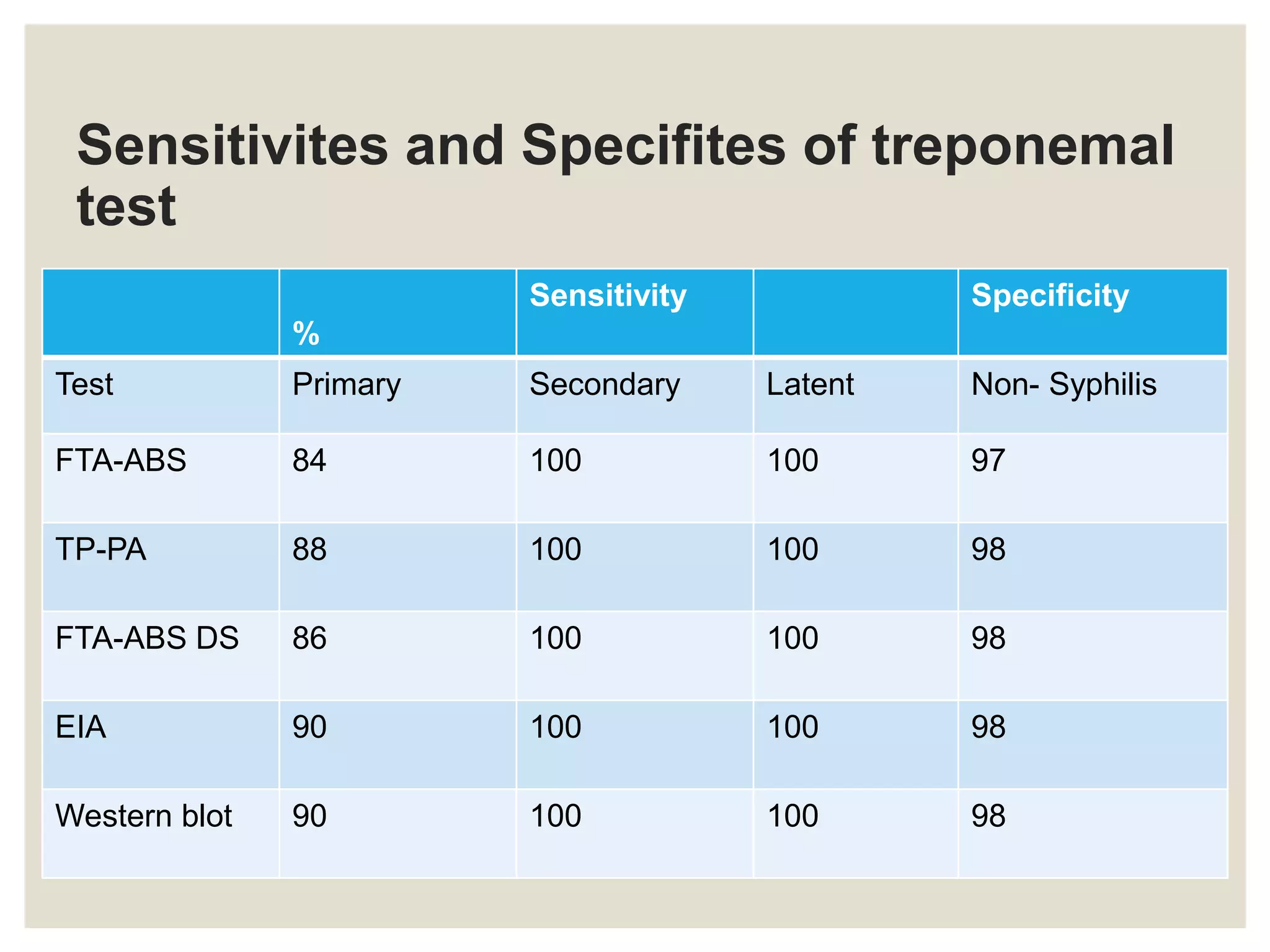
The document discusses Treponema pallidum, the causative agent of syphilis, detailing its history, morphology, pathogenicity, clinical manifestations, laboratory diagnosis, and treatment. It outlines the stages of syphilis, including primary, secondary, latent, and late manifestations, along with congenital syphilis. Additionally, it covers various diagnostic methods, including serologic tests and microscopy techniques, utilized for the detection and diagnosis of syphilis.