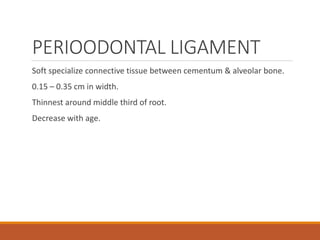
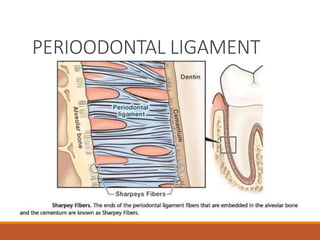
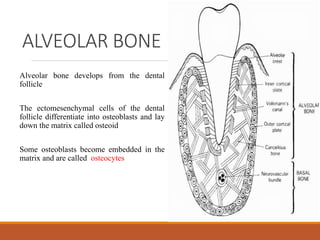
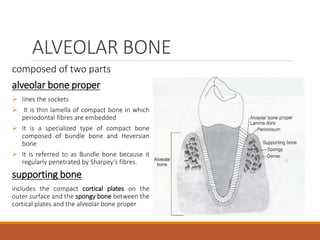
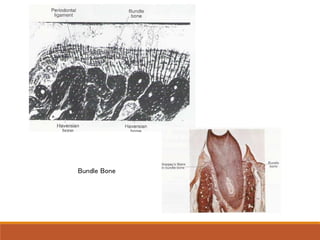
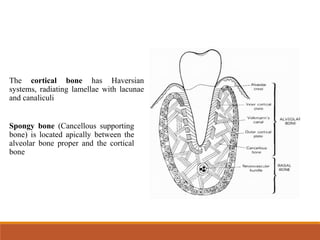
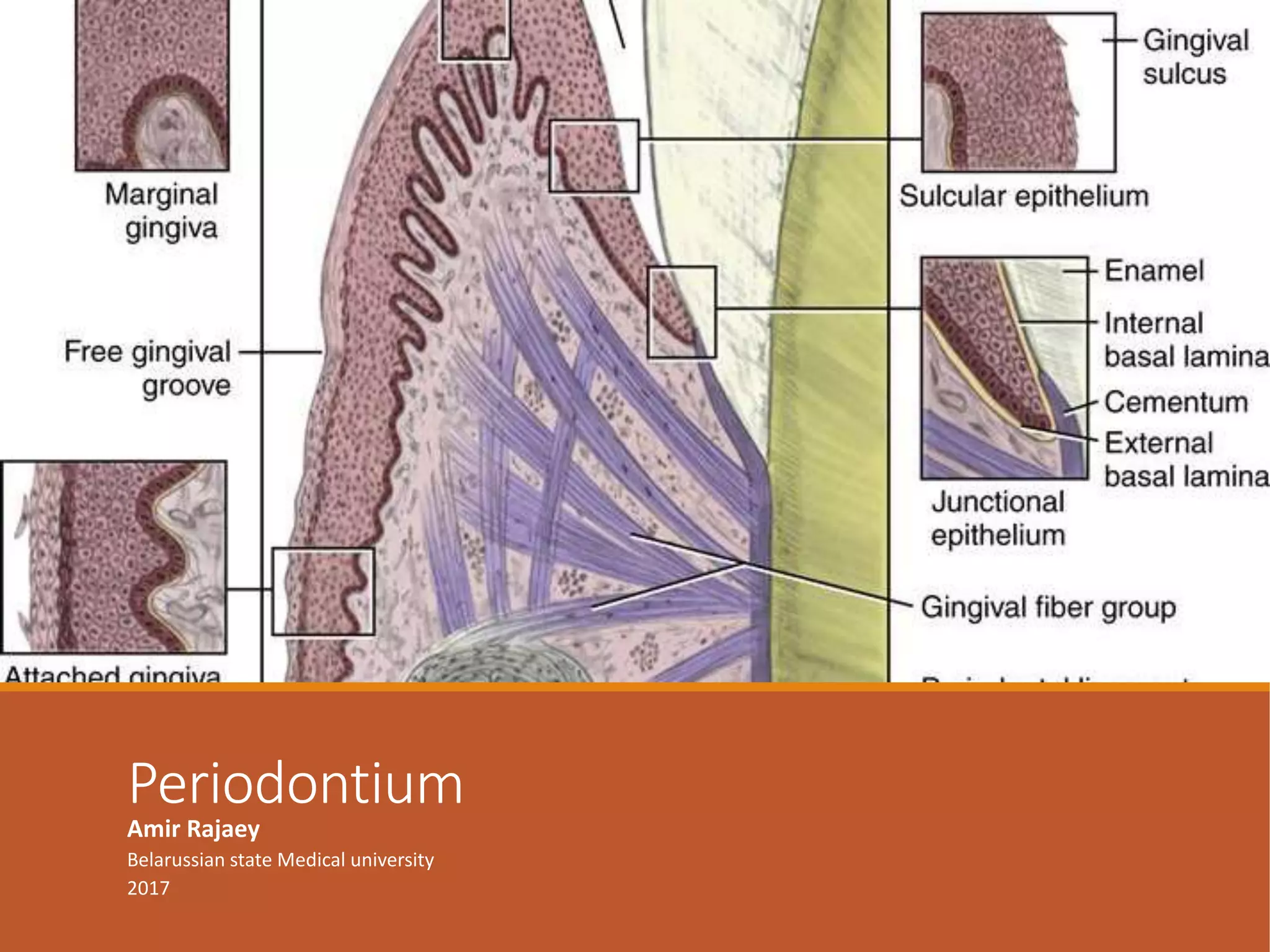
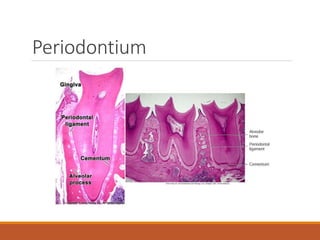
The periodontium consists of cementum, periodontal ligament, alveolar bone, and gingiva. Cementum covers and protects the root dentin. It provides attachment for the periodontal ligament fibers. The periodontal ligament is a soft connective tissue that connects the cementum to the alveolar bone and provides nutrition and sensory function. The alveolar bone surrounds and supports the teeth. It consists of alveolar bone proper and supporting bone.


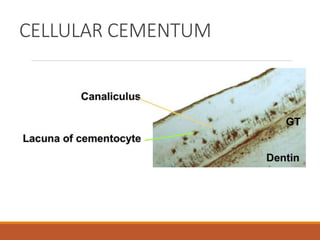
![Secondary cellular cementum
• Both intrinsic and extrinsic fibers
[Extrinsic (5 – 7 µm) and Intrinsic (1 – 2 µm)]
• Bulk of secondary cementum
• Cementocytes
• Laminated structure
• Cementoid on the surface
• Apical portion and intrerradicular area
• Adaptation
Intrinsic fibers are uniformly mineralized but the extrinsic fibers are
variably mineralized with some central unmineralized cores](https://image.slidesharecdn.com/periodontium3-170113140724/85/Periodontium-18-320.jpg)