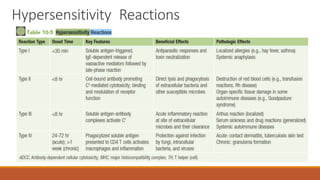
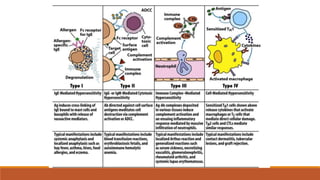
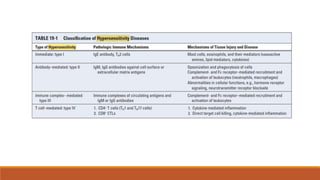
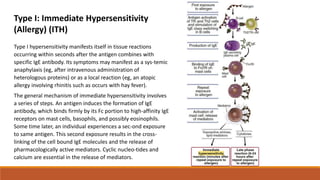
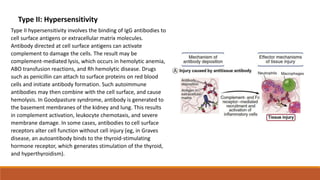
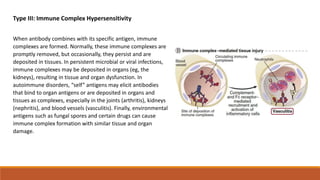
Hypersensitivity is an exaggerated immune response harmful to the host, occurring typically after re-exposure to a specific antigen. It includes four types: immediate (Type I), antibody-mediated (Type II), immune complex-mediated (Type III), and T cell-mediated (Type IV), each with distinct mechanisms and clinical manifestations. Conditions can range from allergies and autoimmune diseases to tissue damage due to immune complex deposition.


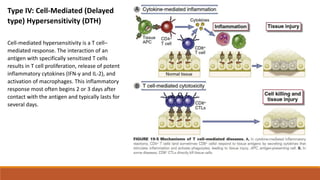
![Type IV hypersensitivity: delayed-type hypersensitivity (DTH) mediated by CD4 T cells (TH1). In this case, chemically
modified self-proteins are processed, and peptides are presented to CD4 memory T cells cycling through the skin,
which release cytokines (including interferon-γ [IFN-γ]) that promote inflammation. Other examples of DTH are the
tuberculin response (purified protein derivative test) and reaction to metals such as nickel. APC, Antigen-presenting
cell; TCR, T-cell receptor.](https://image.slidesharecdn.com/hypersensitivity-170619195910/85/Hypersensitivity-8-320.jpg)