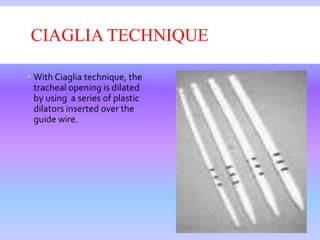
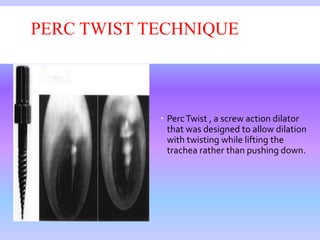
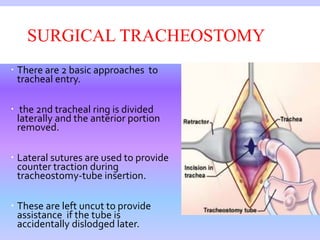
The document provides a comprehensive overview of tracheostomy procedures, including definitions, historical context, indications, and various surgical techniques. It details the anatomy involved, types of tracheostomy tubes, potential complications, and care measures following the procedure. Additionally, it discusses weaning and speech rehabilitation options for patients with tracheostomies.