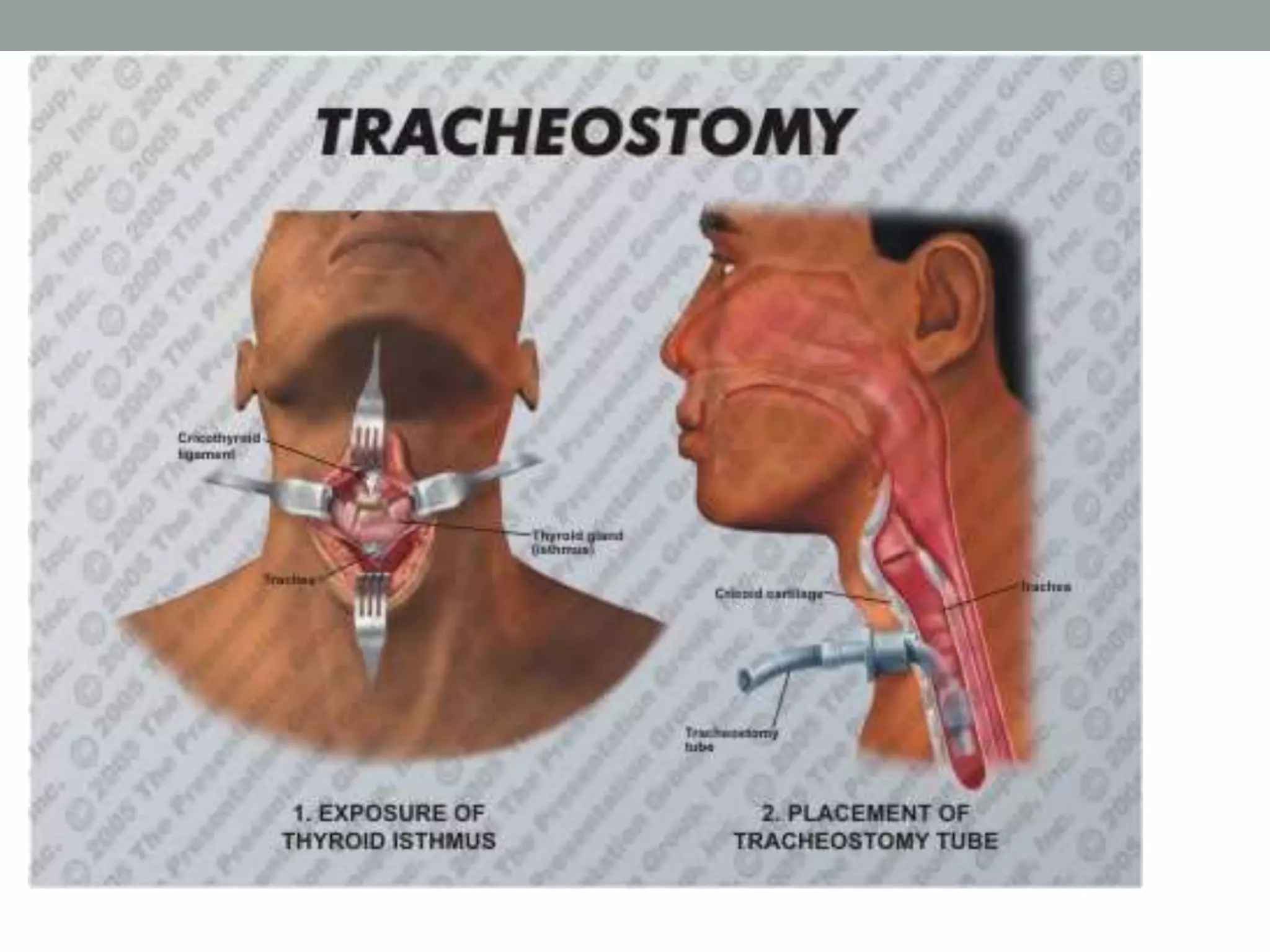
Tracheostomy is an opening created in the trachea to allow for an alternative airway. It provides benefits like improved breathing, secretion removal, and ventilation assistance. Tracheostomies are indicated for respiratory obstruction, retained secretions, or respiratory insufficiency. The procedure involves making an incision through the neck and trachea to insert a tube. Post-op care includes tube maintenance and cleaning to prevent complications like infection, stenosis, or fistula formation. Decannulation is the process of removing the tube when the underlying condition has resolved.