Central serous chorioretinopathy (CSCR) is characterized by spontaneous serous detachment of the neurosensory retina in the macular region. It typically affects young to middle-aged males and is associated with type A personality and steroid use. The leading pathogenesis theory is choroidal vascular hyperpermeability causing a breach in the outer blood-retinal barrier and leakage of fluid. On examination, CSCR presents as mild macular elevation with or without retinal pigment epithelium detachment. It usually resolves spontaneously but can recur in 30-50% of cases.
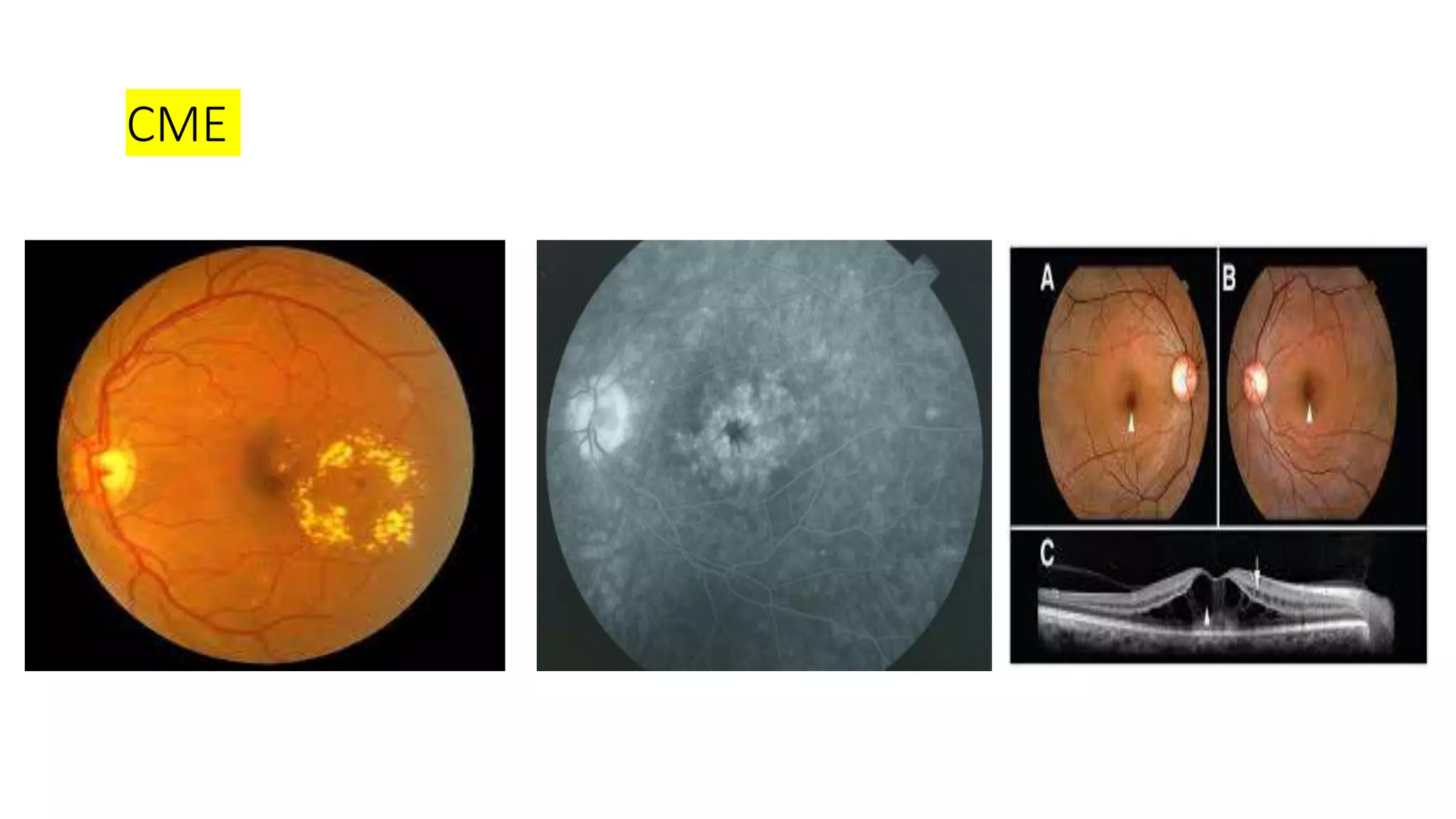
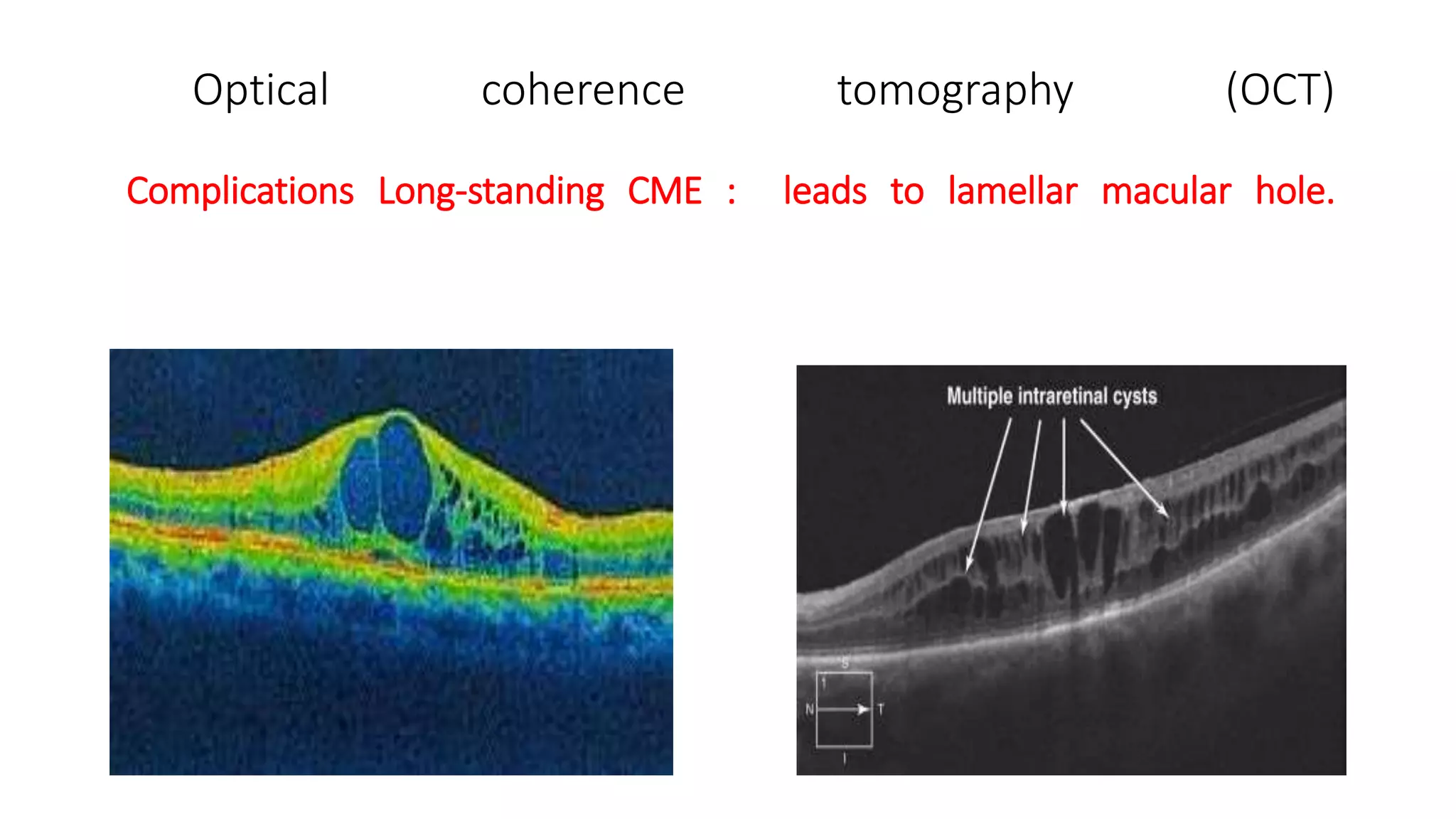
Cystoid macular edema (CME) refers to fluid collection in the macula and is a complication of ocular surgery,
















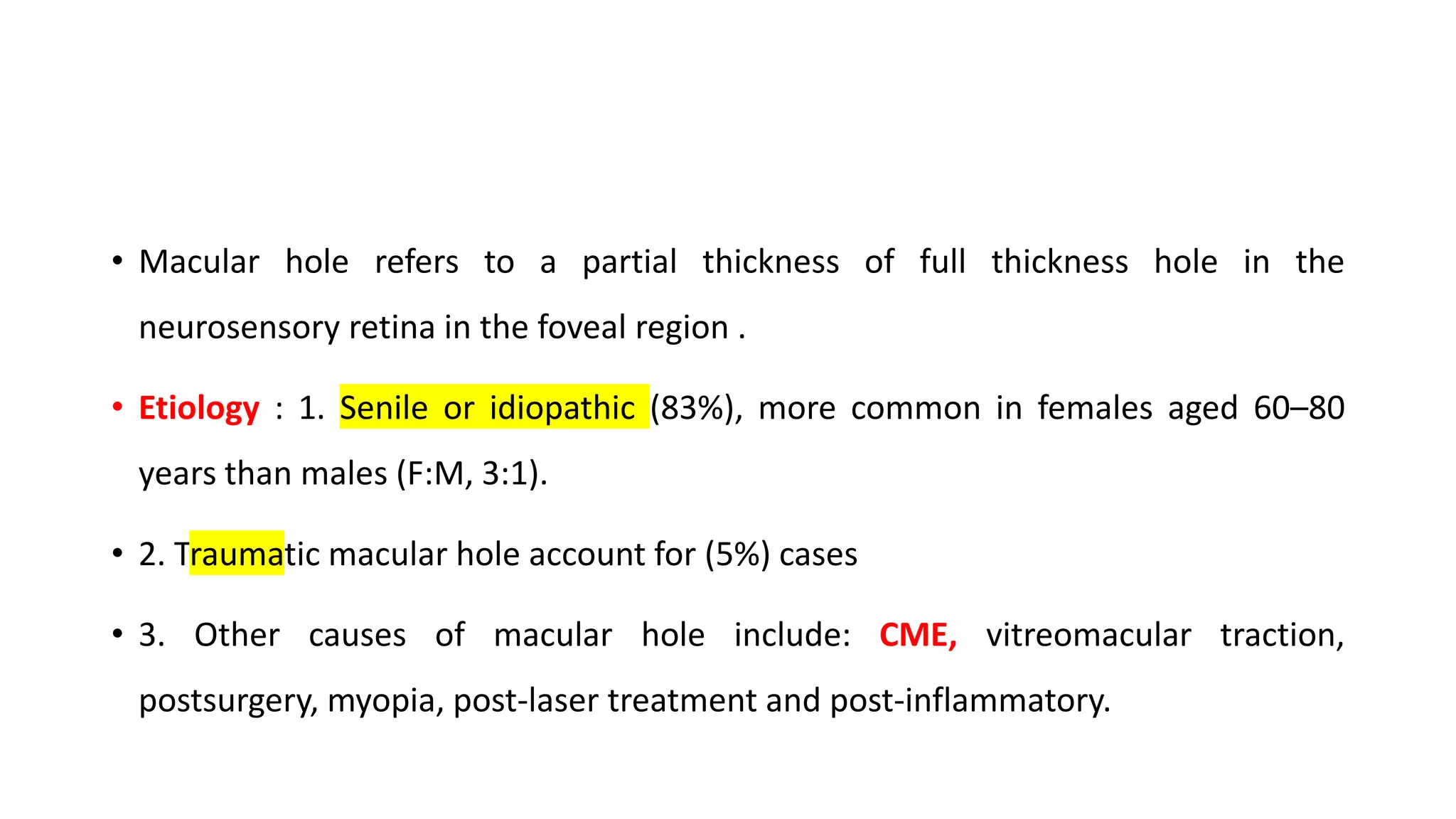



![• Stage 1 or impending hole : it shows absent foveal reflex & a yellow spot or
yellow ring in the foveal region .
• Stage 2. A small full thickness hole ( either centre or marginal ) full thickness hole
less than 400 um in size
• Stage 3. A full thickness hole is seen as round reddish spot surrounded by a grey
halo [cuff of subretinal fluid (SRF)]& no PVD ,more than 400 um in size
• Stage 4. Full thickness hole with with posterior vitreous detached from the disc
and macula .](https://image.slidesharecdn.com/cscrcentralserouschorioretinopathy-200310100316/75/Cscr-central-serous-chorioretinopathy-26-2048.jpg)





