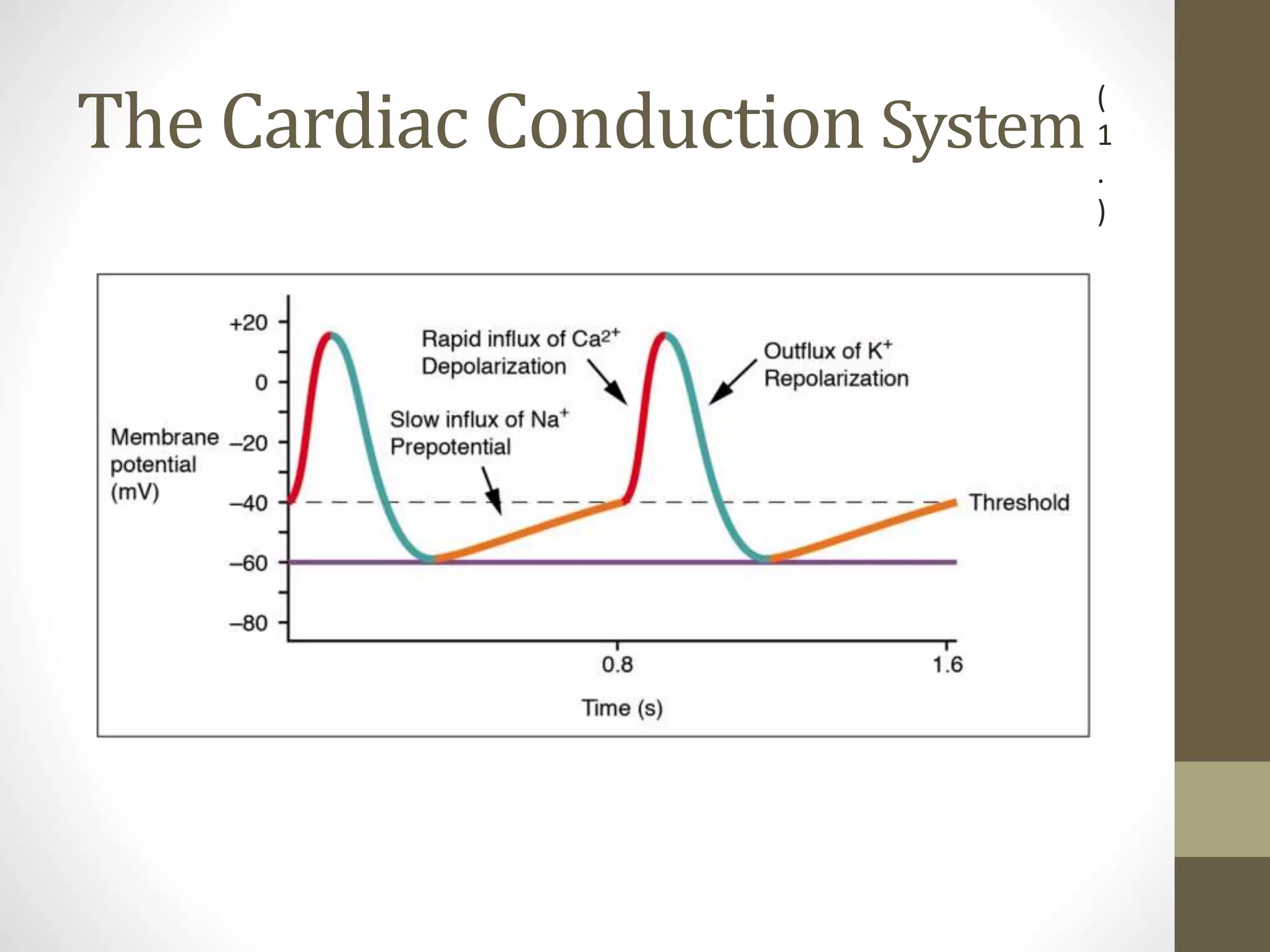
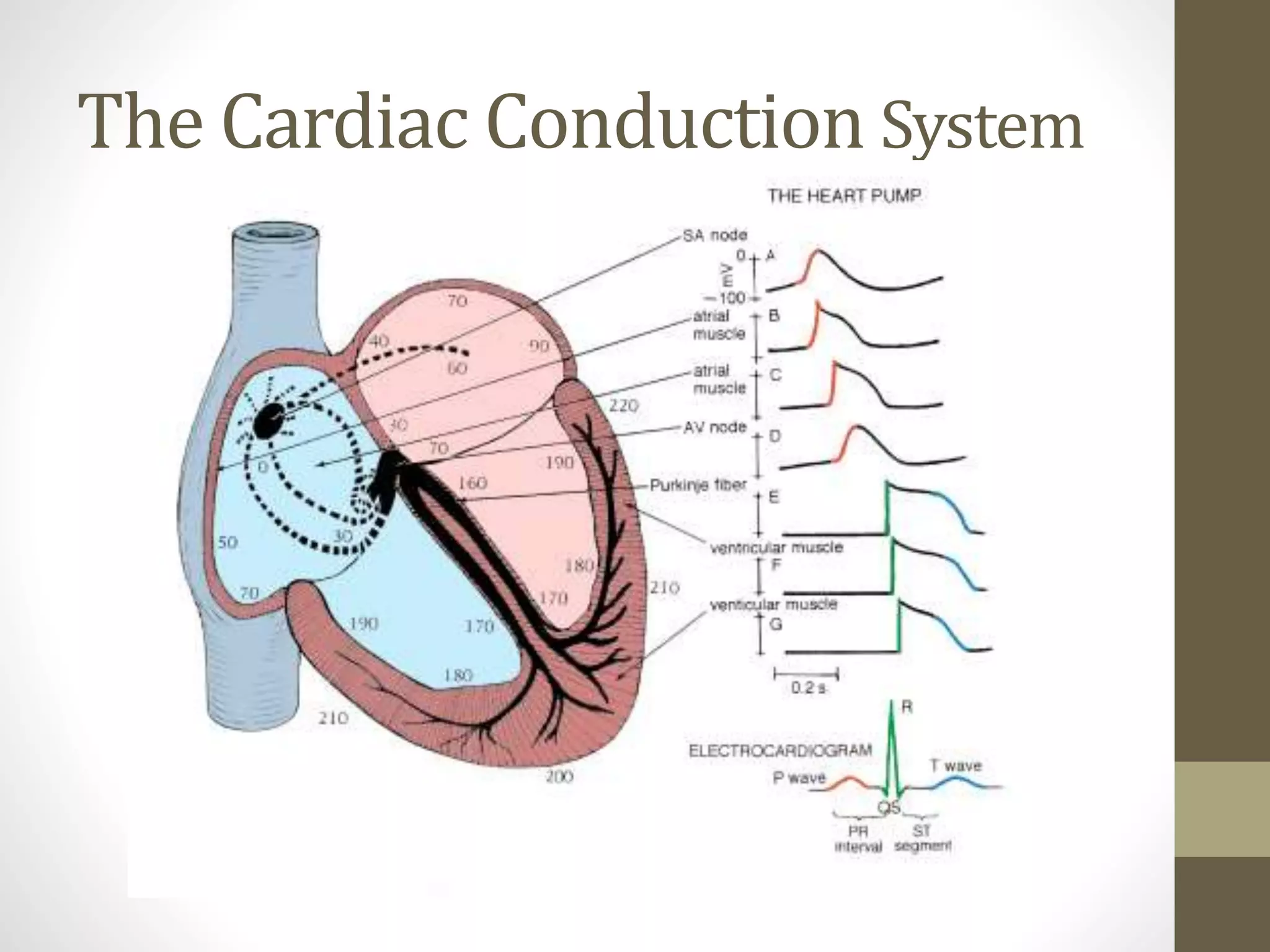
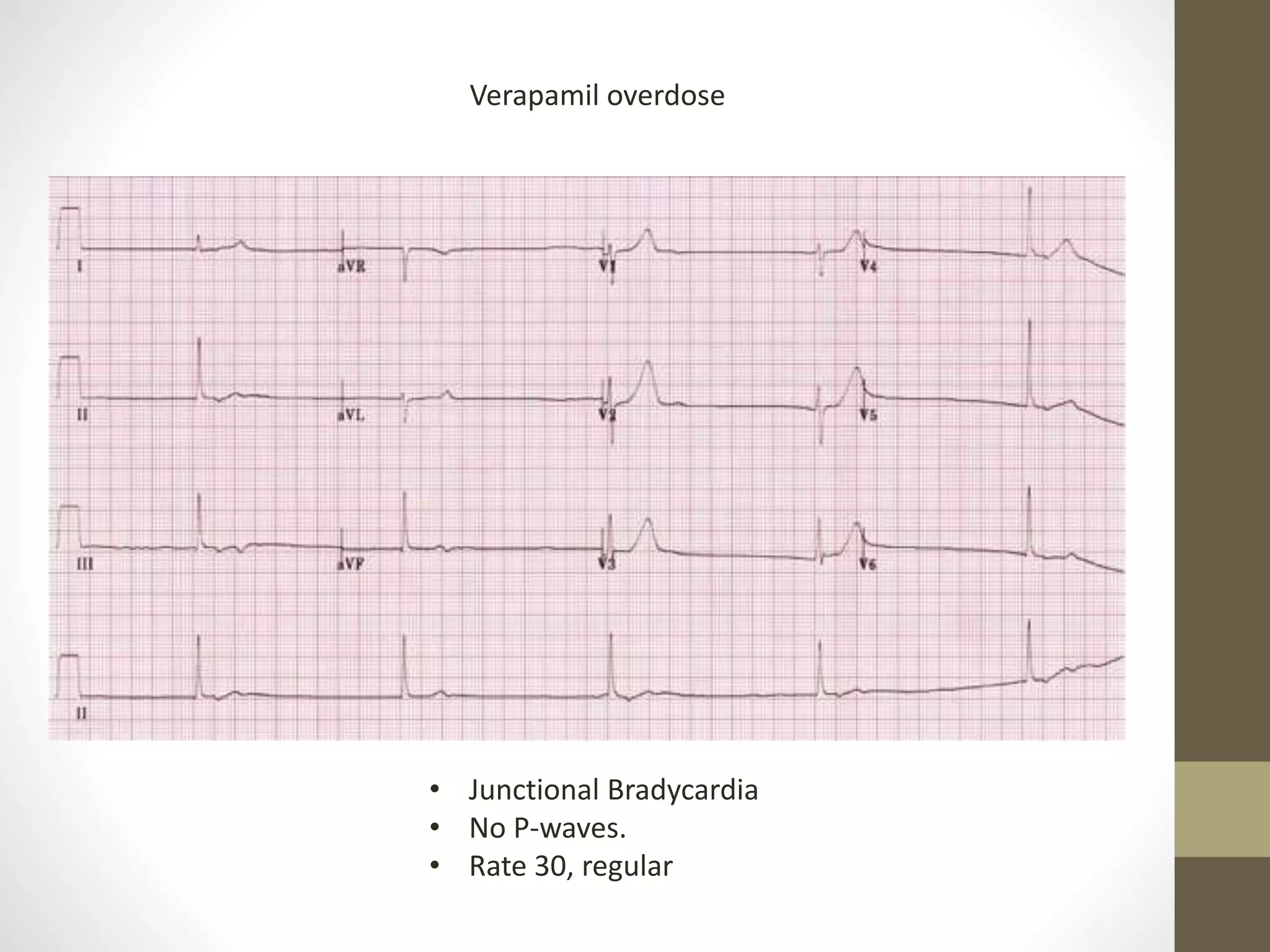
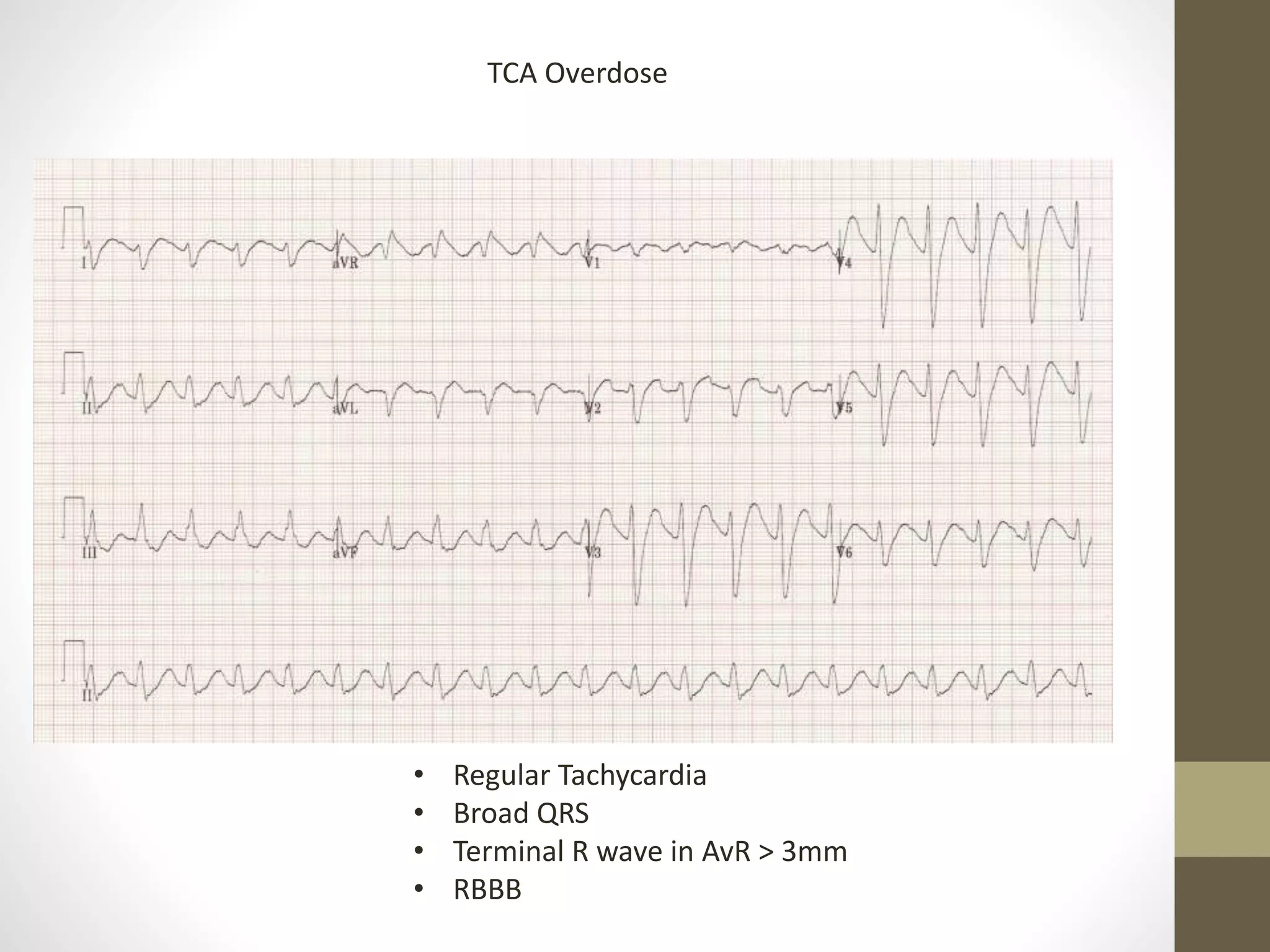
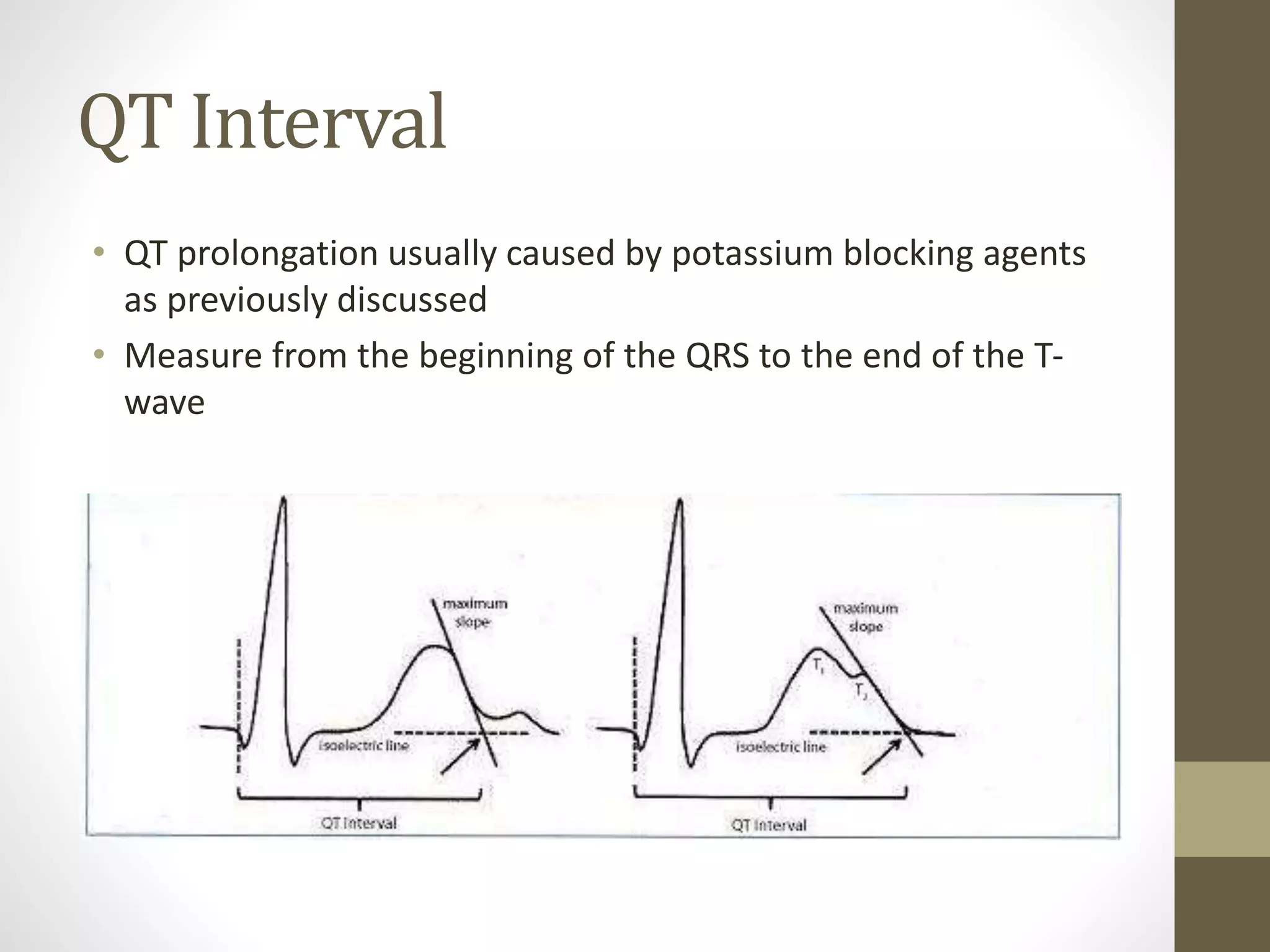
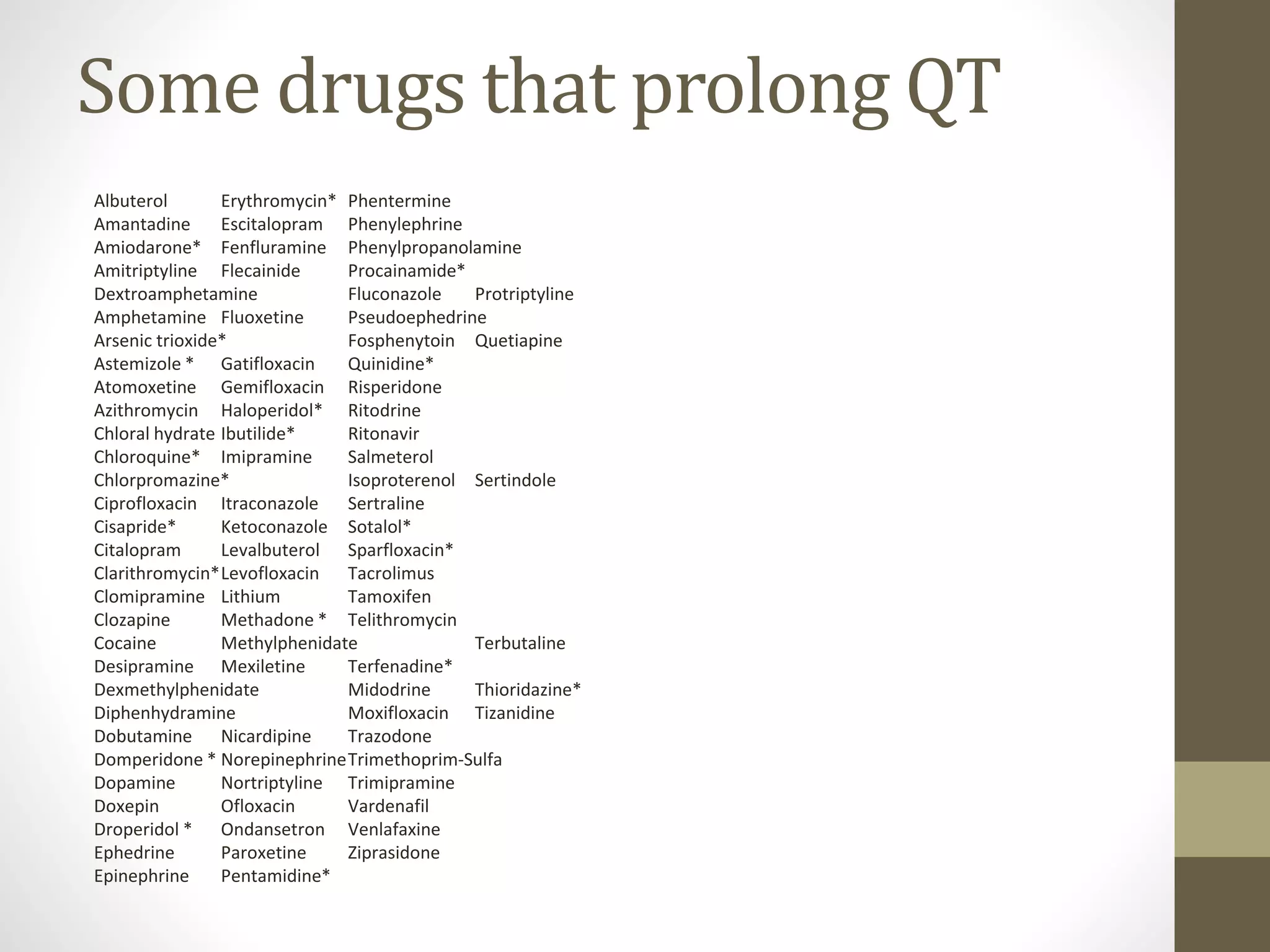
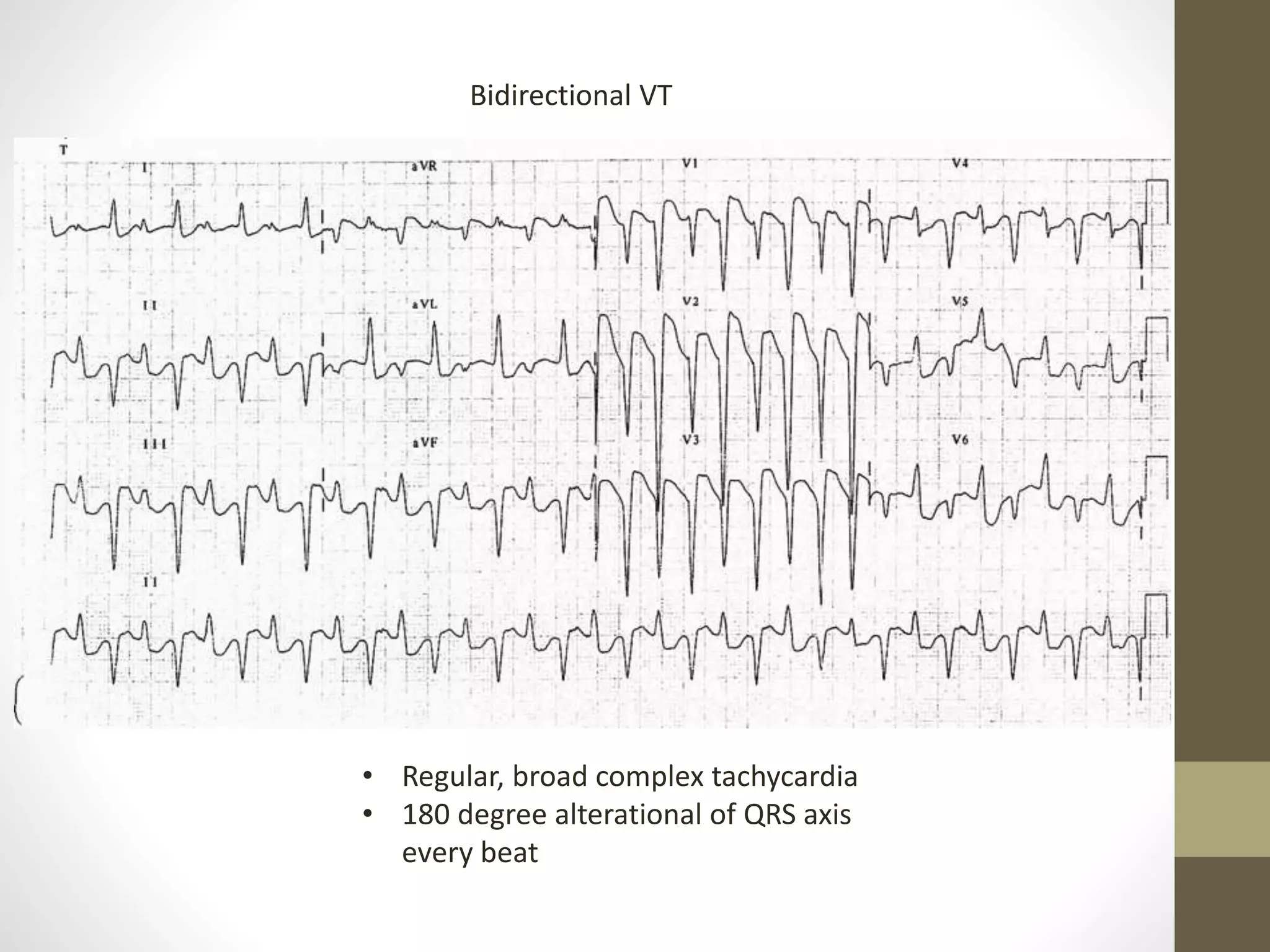
This document discusses toxicology and ECG interpretation in poisoned patients. It provides an overview of the cardiac conduction system and how specific drugs can affect it. Drugs that block sodium channels can cause a wide QRS complex, while potassium channel blockers prolong the QT interval and increase risk of Torsades de Pointes. A systematic approach to ECG interpretation is outlined, examining rate, rhythms, intervals, and morphology. Management strategies are presented for various cardiotoxic drugs like beta blockers, calcium channel blockers, sodium channel blockers, and cardiac glycosides.