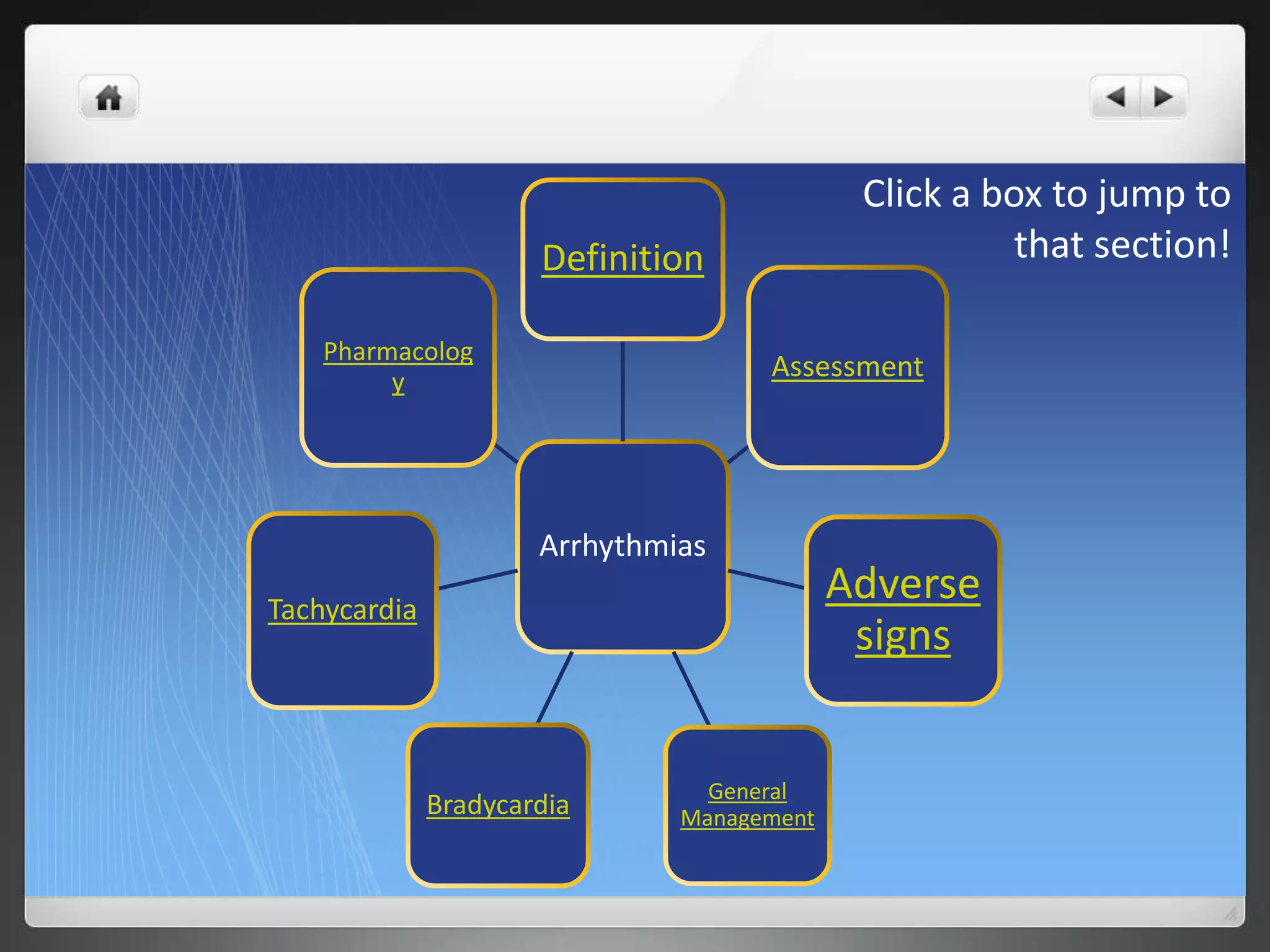
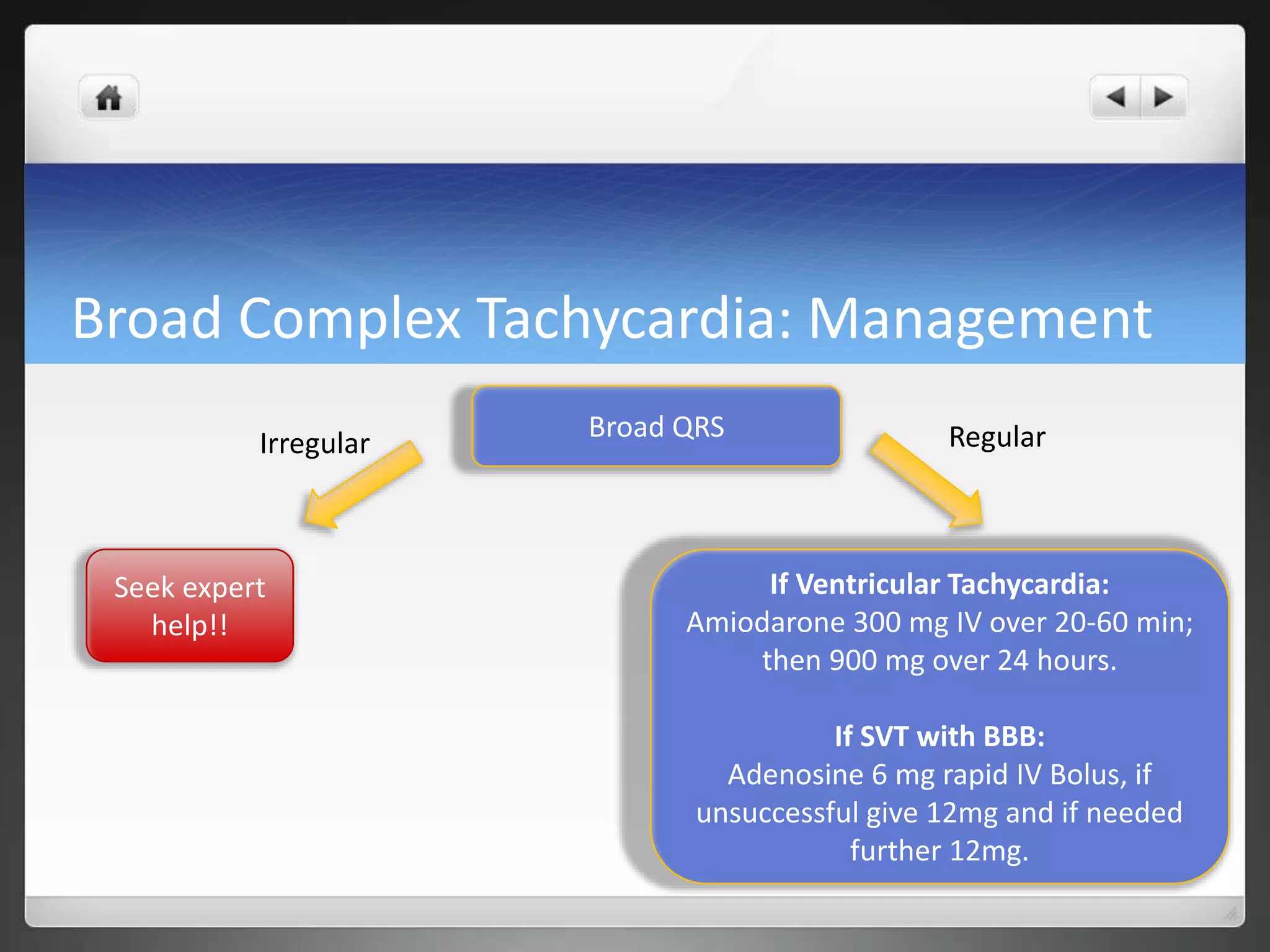
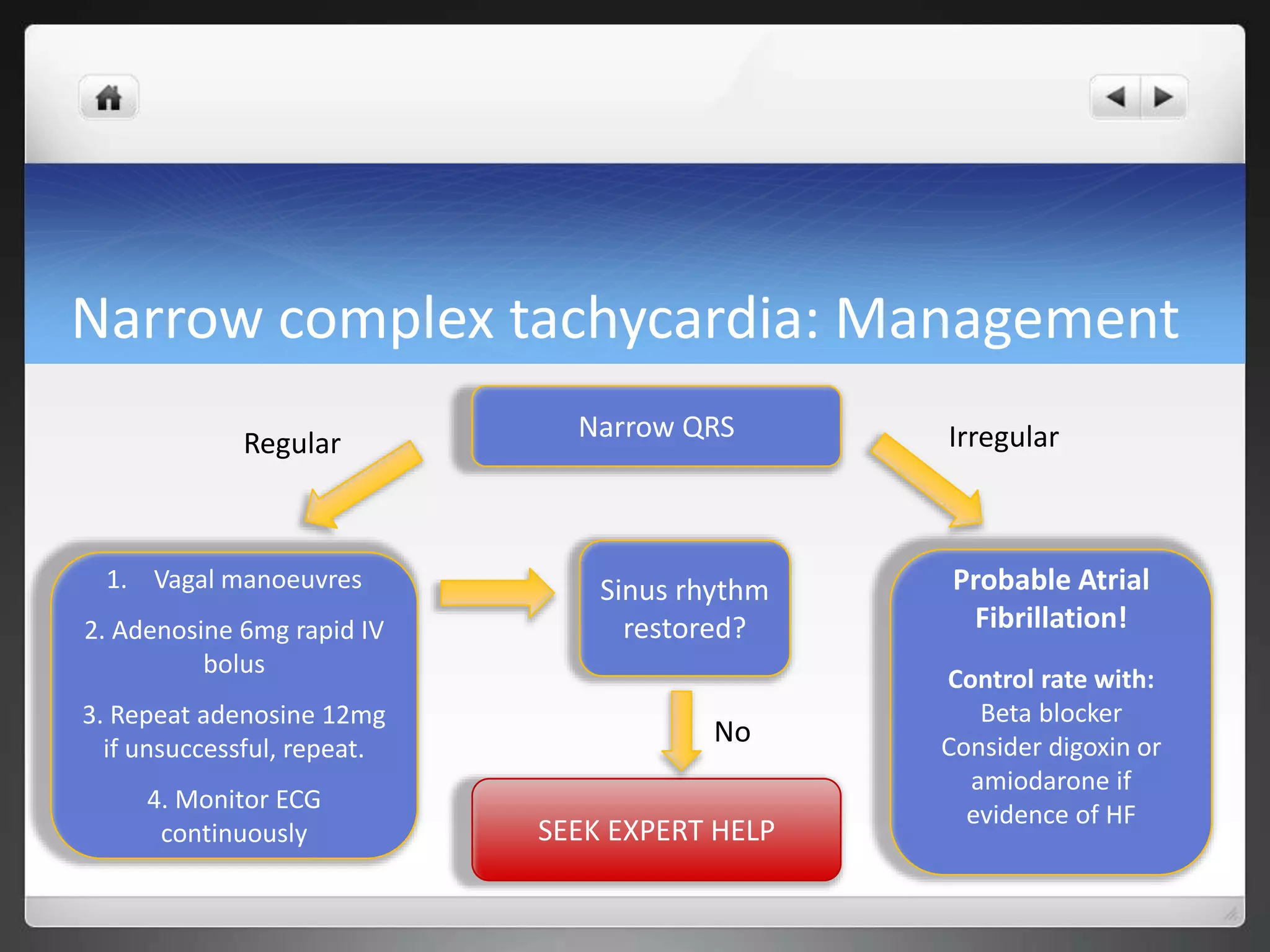
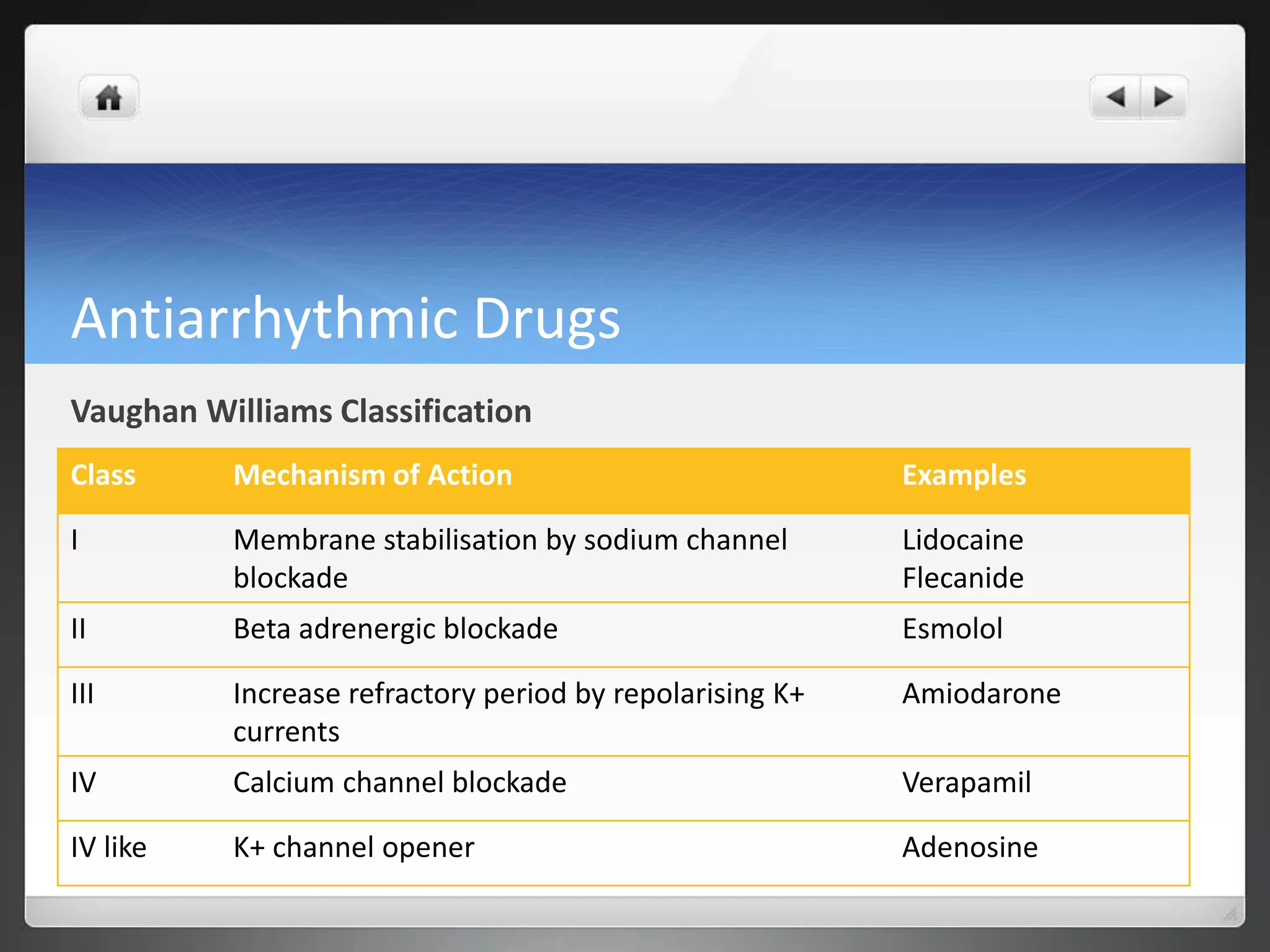
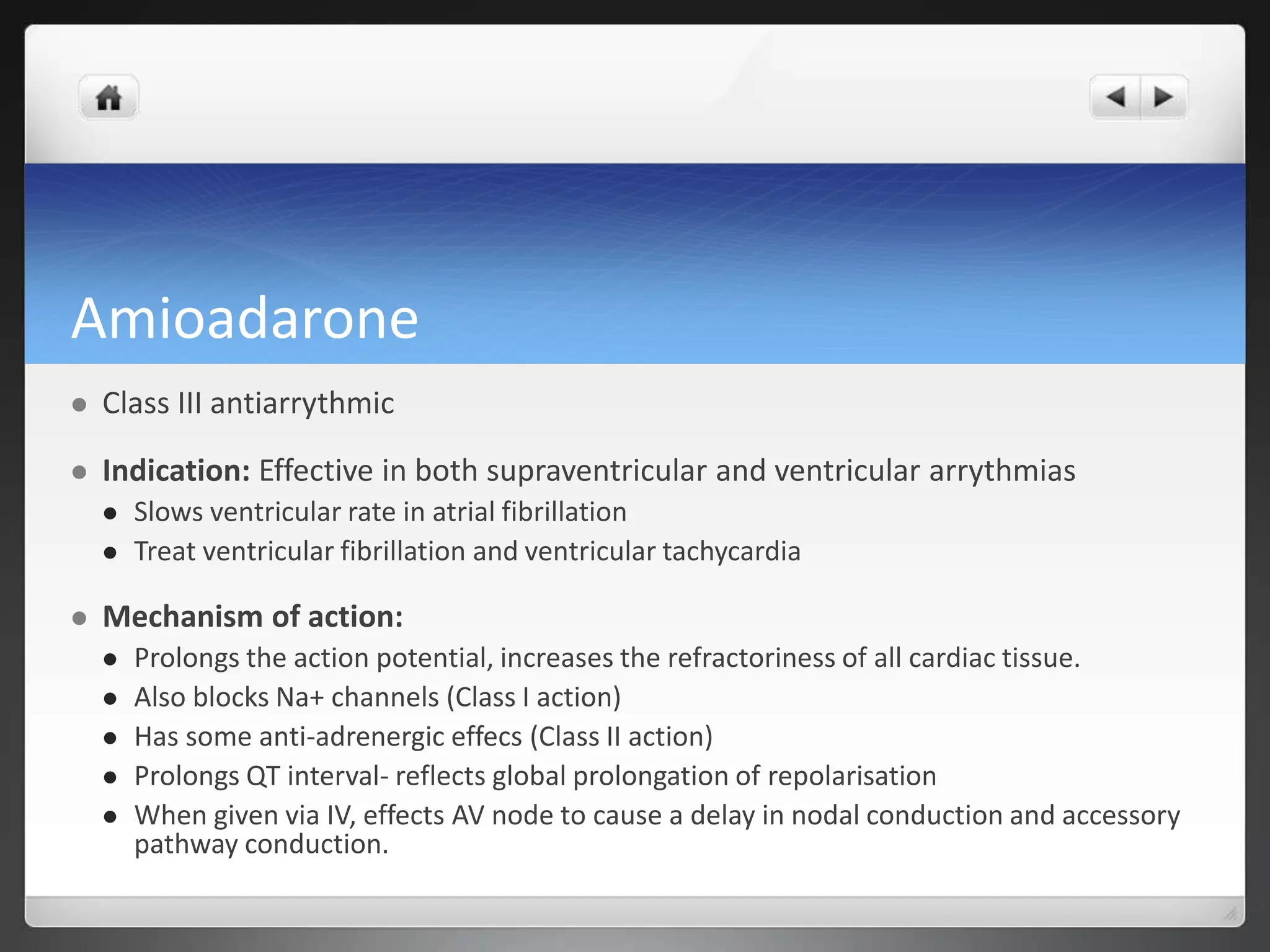
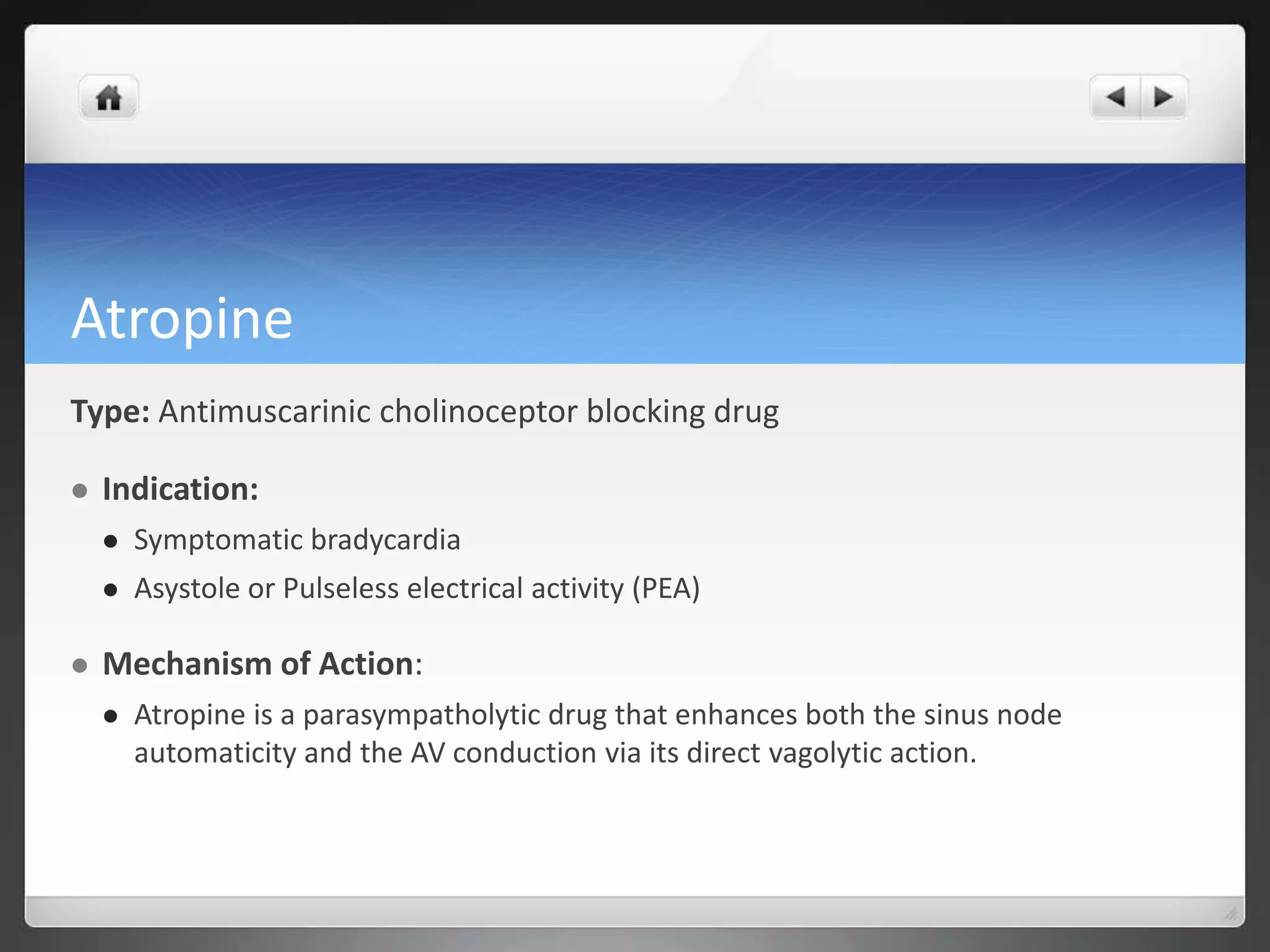
This document discusses the management of peri-arrest arrhythmias. It defines arrhythmias and describes their assessment and general treatment options. It covers the management of specific arrhythmias like bradycardia and tachycardias. It also discusses the pharmacology of common antiarrhythmic drugs like amiodarone, atropine, digoxin. The document provides guidelines on stabilizing patients and restoring normal heart rhythm in peri-arrest settings.