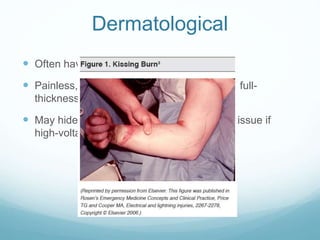
This document provides an overview of electrical injuries, including pathophysiology, types, organ effects, management in the emergency department, and common pitfalls. It discusses how the extent of tissue damage from electrical injuries depends on voltage, current, resistance, and duration of contact. Management involves treating for potential cardiac, respiratory, neurological, musculoskeletal and dermatological effects. High voltage or low voltage injuries with concerning findings require admission. Delays effects like cataracts or bleeding can occasionally occur.