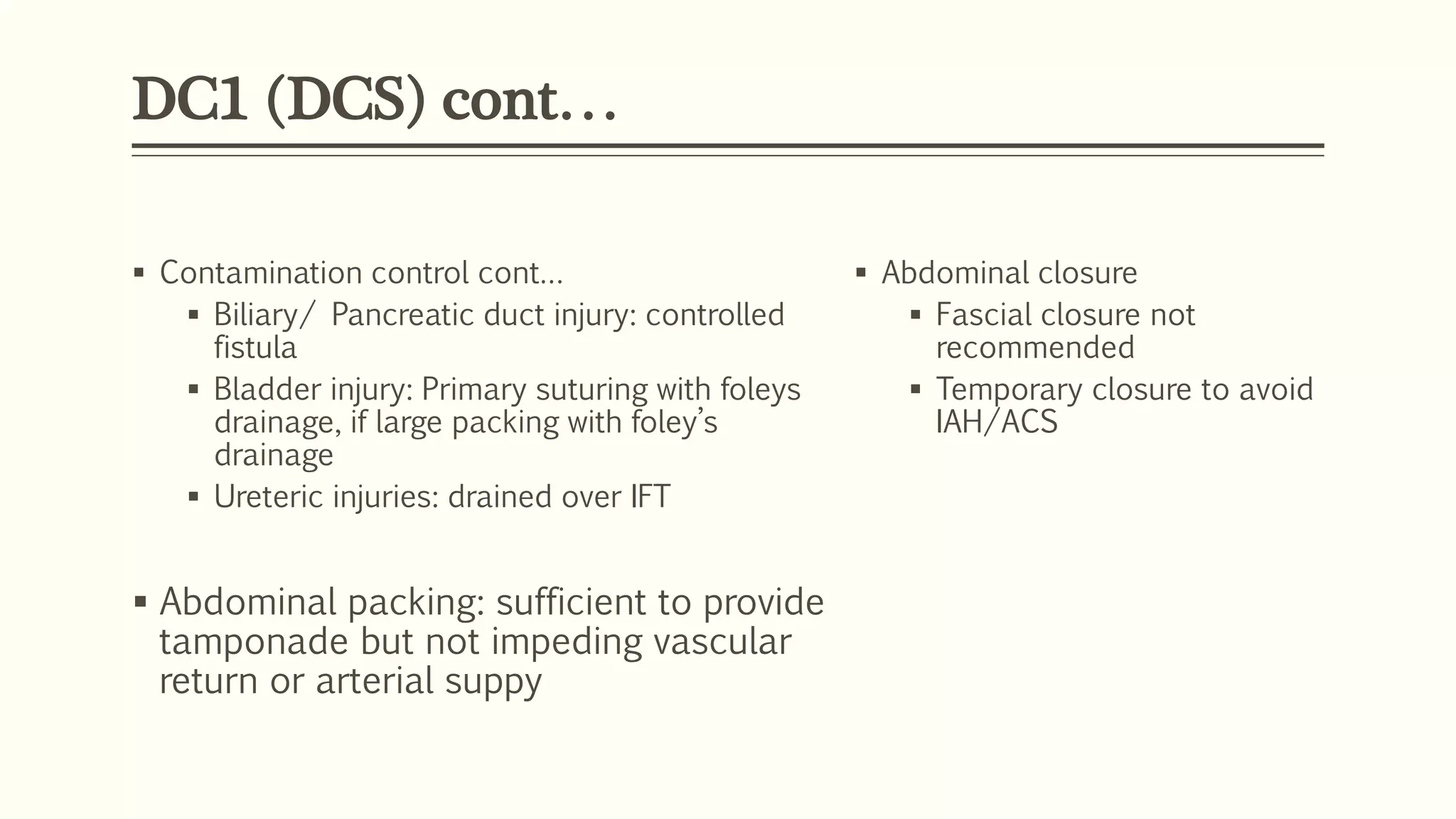
Damage control surgery (DCS) is a strategy that prioritizes physiological recovery over anatomical repair for critically injured patients. It follows a four phase approach: DC0 involves damage control resuscitation in the field and emergency room; DC1 is concurrent resuscitation and surgery to control hemorrhage through packing and temporary closure; DC2 focuses on intensive care stabilization and reversal of acidosis, hypothermia and coagulopathy; DC3 performs definitive repair once physiology is normalized within 24-36 hours. DCS indications include massive transfusion, severe acidosis, hypothermia, long operative times, coagulopathy and high lactate levels.