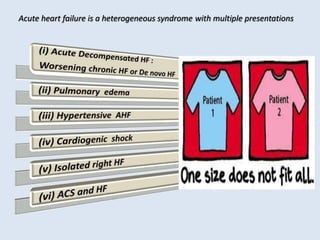
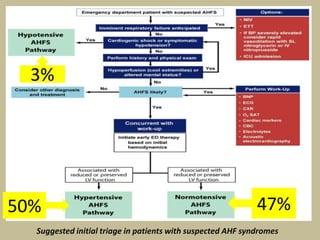
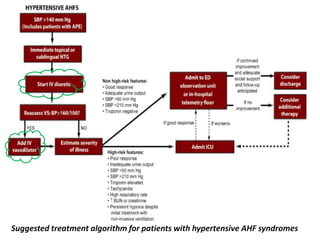
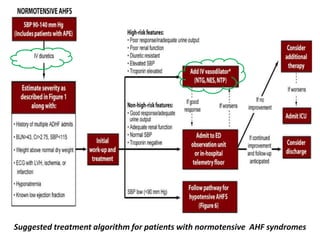
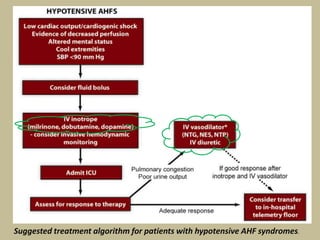
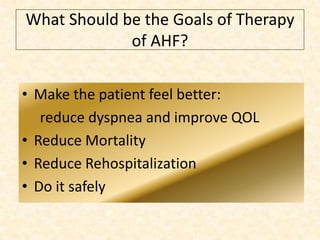
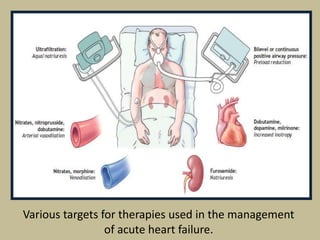
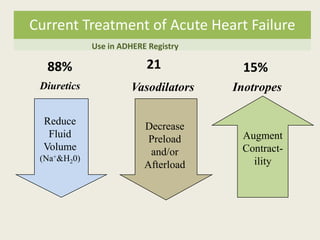
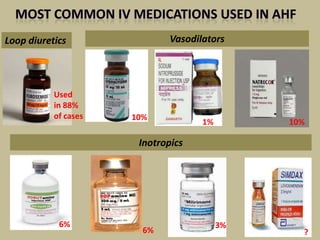
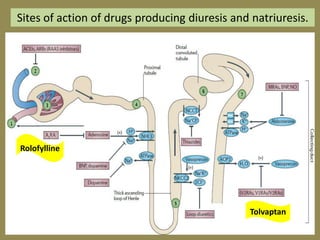
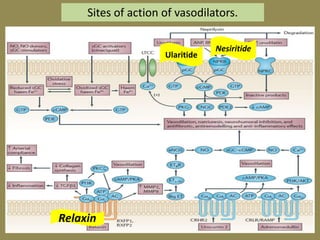
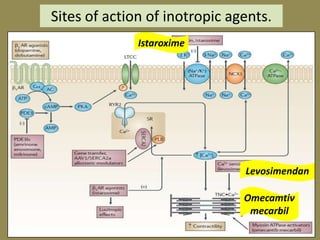
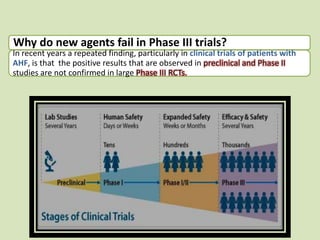
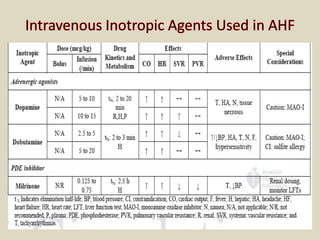
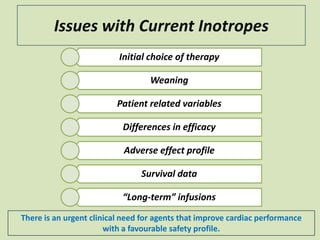
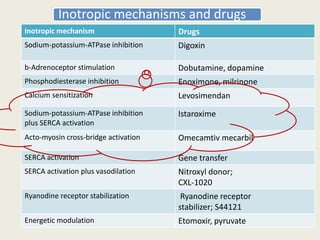
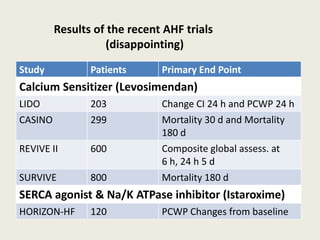
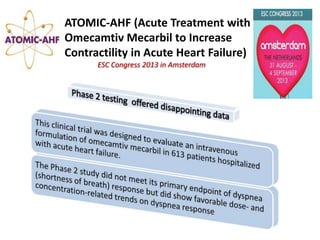
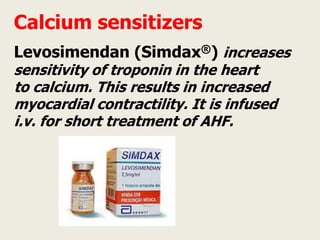
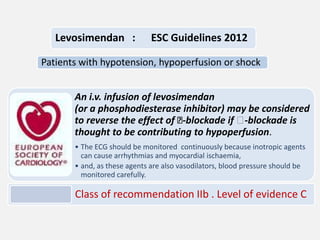
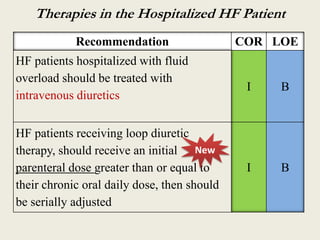
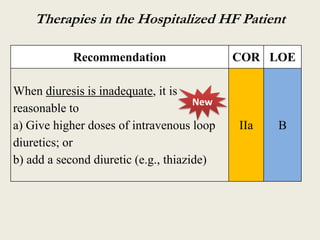
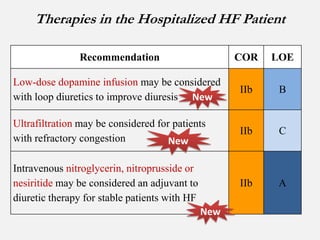
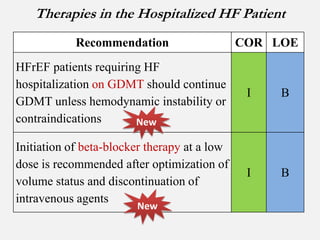
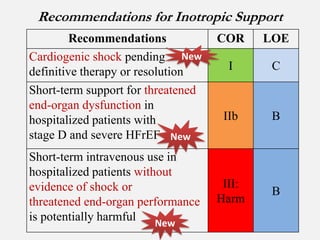
This document provides guidelines for the management of acute heart failure. It discusses current treatment strategies including diuretics, vasodilators, and inotropes. Novel therapeutic strategies are mentioned, such as newer inotropic drugs, rollofylline, tolvaptan, ularitide, relaxin, and others. The goals of therapy for acute heart failure are to make the patient feel better by reducing dyspnea, improve quality of life, reduce mortality and rehospitalization, and do so safely. Recent large clinical trials of new agents for acute heart failure have failed to show benefits observed in smaller earlier studies.