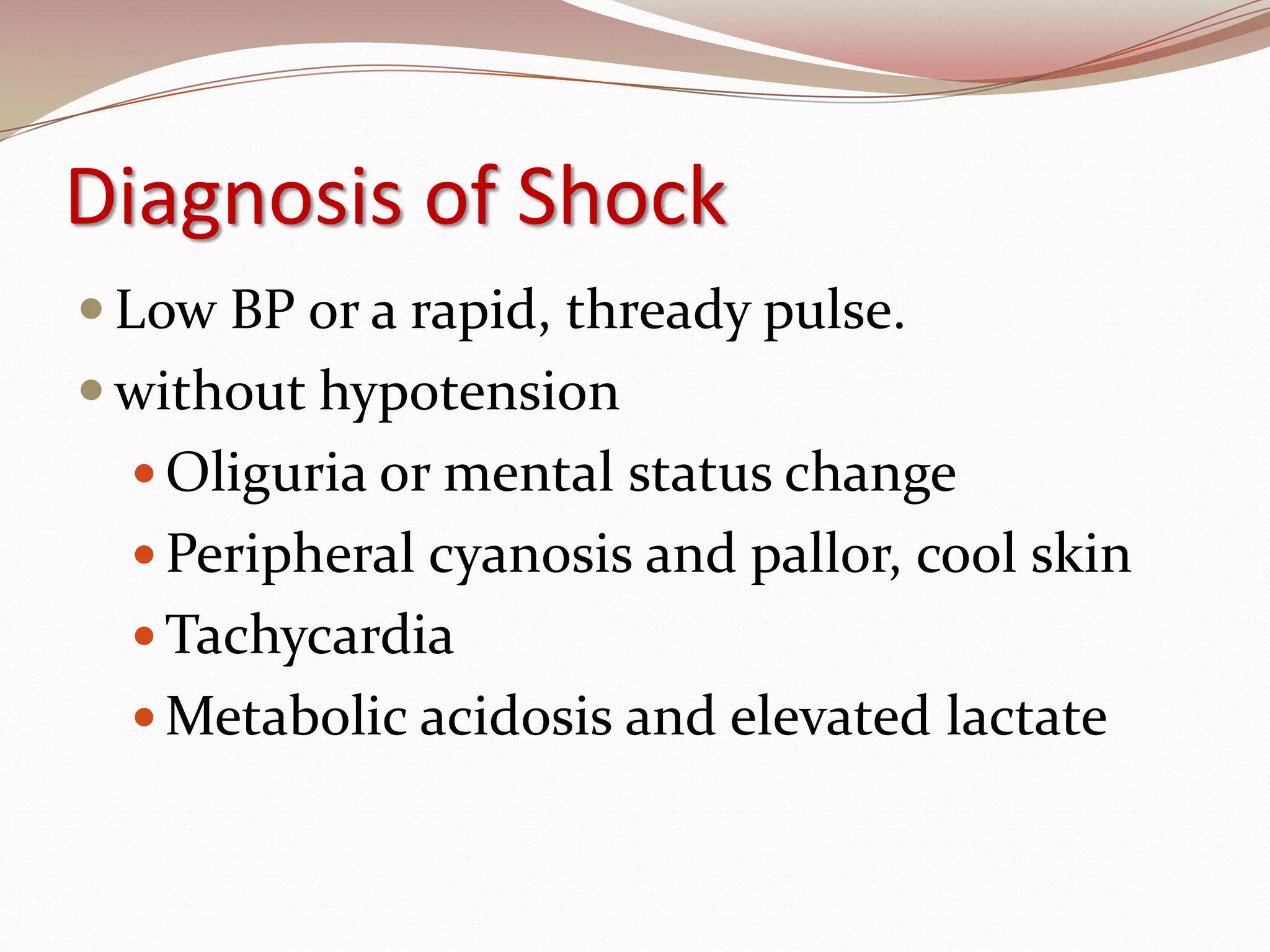
The document discusses shock pathophysiology and management. It defines shock as inadequate tissue perfusion leading to hypoxia. Oxygen delivery is determined by cardiac output and hemoglobin/oxygen saturation levels. The types of shock are classified as hypodynamic or hyperdynamic based on cardiac output. Treatment involves fluid resuscitation and vasopressors to support perfusion as needed.






![Oxygen Delivery (DO2) = Cardiac Output x Oxygen Content = CO x [(1.3 x Hb x SaO 2 ) + (0.003 x PaO 2 )] Hb concentration CO SaO 2 % of O 2 in artery PaO 2 (minimal) pressure of O 2 in artery Inadequate DO 2 occurs most often because of low cardiac output](https://image.slidesharecdn.com/1855621/75/Approach-to-Shock-and-Hemodynamics-11-2048.jpg)

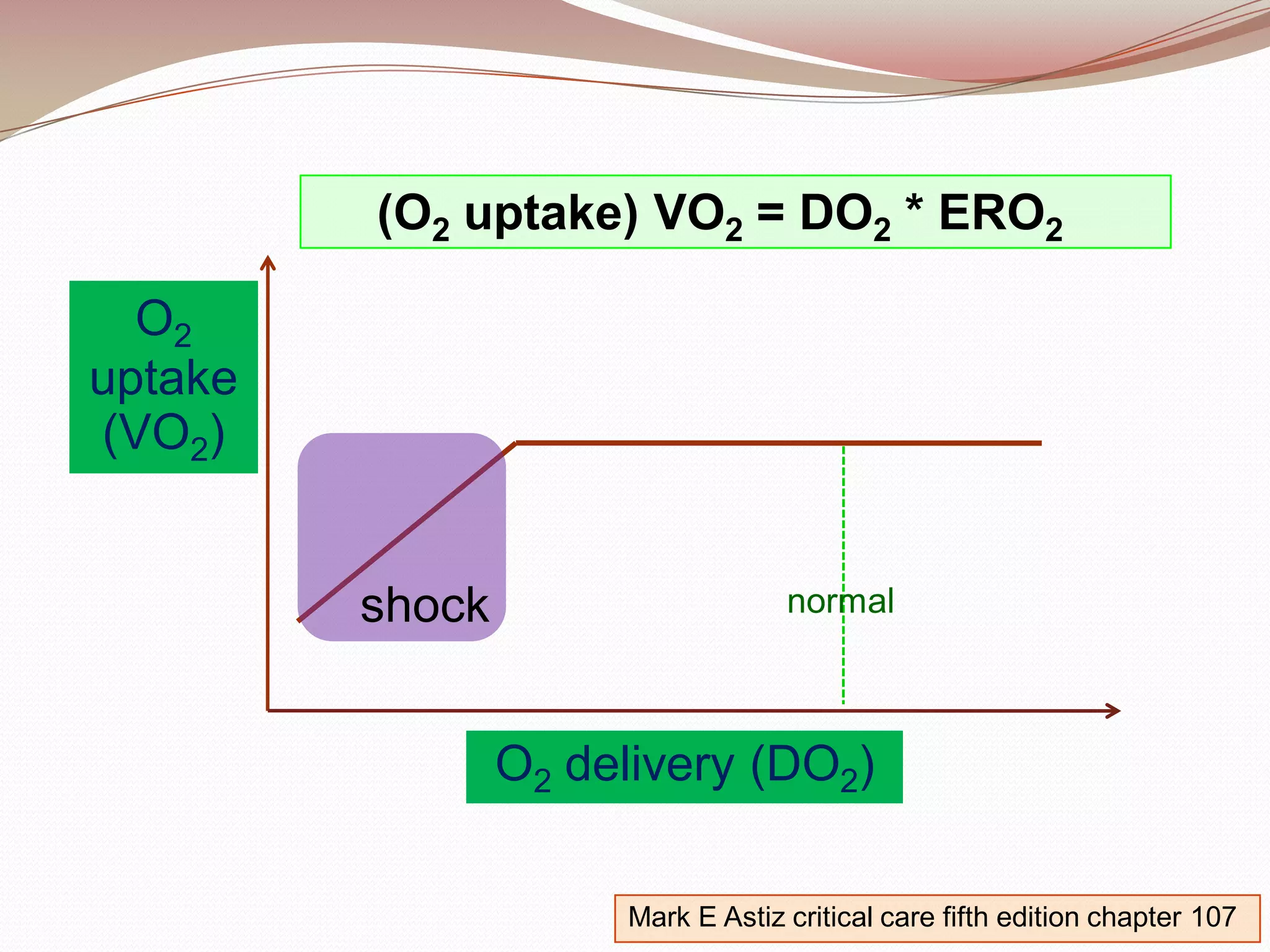
![Conclusion Shock lead to tissue hypoxia Oxygen uptake (VO 2 ) < Oxygen demand O 2 uptake (VO 2 ) = O2 delivery (DO2) * O2 extraction ratio (ERO2) O2 delivery (DO2) = Cardiac Output x Oxygen Content = [SV x HR] x [(1.3 x Hb x SaO 2 ) + (0.003 x PaO 2 )] SV ~ (Preload * Contractility) / Afterload](https://image.slidesharecdn.com/1855621/75/Approach-to-Shock-and-Hemodynamics-13-2048.jpg)

![Classification of shock Hypodynamic hypovolemic (hemorrhagic , nonhemorrhagic) cardiogenic obstructive ( PE,cardiac temponade ,tension pneumothorax) Mark E Astiz critical care fifth edition chapter 107 O2 delivery (DO2) = Cardiac Output x Oxygen Content = [SV x HR] x [(1.3x Hb x SaO 2 ) + (0.003x PaO 2 )] SV ~ Preload * Contractility Afterload](https://image.slidesharecdn.com/1855621/75/Approach-to-Shock-and-Hemodynamics-15-2048.jpg)
![Classification of shock Hypodynamic hypovolemic (hemorrhagic, nonhemorrhagic ) cardiogenic obstructive ( PE,cardiac temponade ,tension pneumothorax) Mark E Astiz critical care fifth edition chapter 107 O2 delivery (DO2) = Cardiac Output x Oxygen Content = [SV x HR] x [(1.3x Hb x SaO 2 ) + (0.003x PaO 2 )] SV ~ Preload * Contractility Afterload](https://image.slidesharecdn.com/1855621/75/Approach-to-Shock-and-Hemodynamics-16-2048.jpg)
![Classification of shock Hypodynamic hypovolemic (hemorrhagic, nonhemorrhagic) cardiogenic obstructive ( PE,cardiac temponade ,tension pneumothorax) Mark E Astiz critical care fifth edition chapter 107 O2 delivery (DO2) = Cardiac Output x Oxygen Content = [SV x HR ] x [(1.3x Hb x SaO 2 ) + (0.003x PaO 2 )] SV ~ Preload * Contractility Afterload](https://image.slidesharecdn.com/1855621/75/Approach-to-Shock-and-Hemodynamics-17-2048.jpg)
![Classification of shock Hypodynamic hypovolemic (hemorrhagic, nonhemorrhagic) cardiogenic obstructive ( PE ,cardiac temponade ,tension pneumothorax) Mark E Astiz critical care fifth edition chapter 107 O2 delivery (DO2) = Cardiac Output x Oxygen Content = [SV x HR] x [(1.3x Hb x SaO 2 ) + (0.003x PaO 2 )] SV ~ Preload (left heart) * Contractility Afterload (right heart)](https://image.slidesharecdn.com/1855621/75/Approach-to-Shock-and-Hemodynamics-18-2048.jpg)
![Classification of shock Hypodynamic hypovolemic (hemorrhagic, nonhemorrhagic) cardiogenic obstructive ( PE, cardiac temponade , tension pneumothorax) Mark E Astiz critical care fifth edition chapter 107 O2 delivery (DO2) = Cardiac Output x Oxygen Content = [SV x HR] x [(1.3x Hb x SaO 2 ) + (0.003x PaO 2 )] SV ~ Preload * Contractility Afterload](https://image.slidesharecdn.com/1855621/75/Approach-to-Shock-and-Hemodynamics-19-2048.jpg)
![Classification of shock Hypodynamic hypovolemic (hemorrhagic, nonhemorrhagic) cardiogenic obstructive ( PE,cardiac temponade , tension pneumothorax ) Mark E Astiz critical care fifth edition chapter 107 O2 delivery (DO2) = Cardiac Output x Oxygen Content = [SV x HR] x [(1.3x Hb x SaO 2 ) + (0.003x PaO 2 )] SV ~ Preload * Contractility Afterload](https://image.slidesharecdn.com/1855621/75/Approach-to-Shock-and-Hemodynamics-20-2048.jpg)




![PMHx : Hyperthyroid [PTU(50)2x2 + Propranolol] She has skipped the medication for nearly 2 weeks. ALL : NKDA FHx : 2 Sisters with diabetes. SHx : Occasional alcohol Regular use of over-the-counter drugs (for relieving pain, fatigue and muscle strain)](https://image.slidesharecdn.com/1855621/75/Approach-to-Shock-and-Hemodynamics-27-2048.jpg)