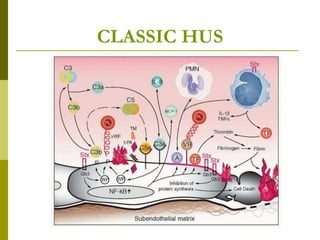
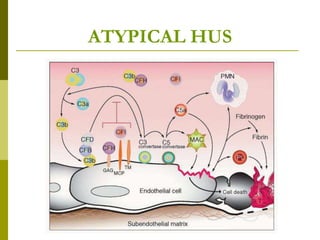
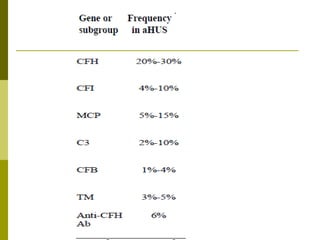
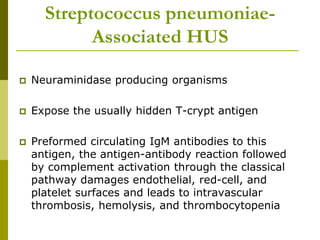
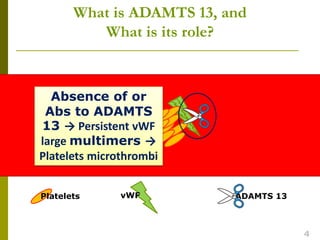
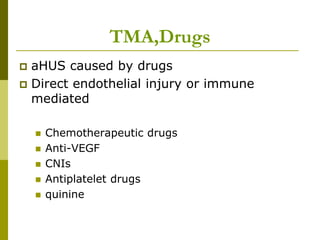
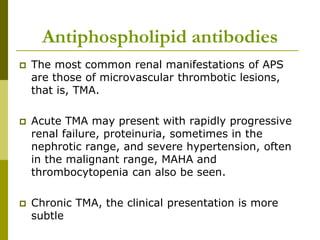
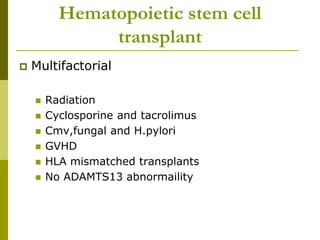
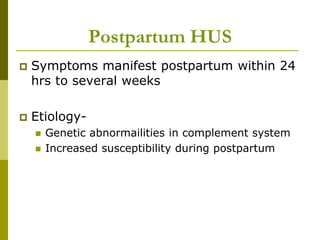
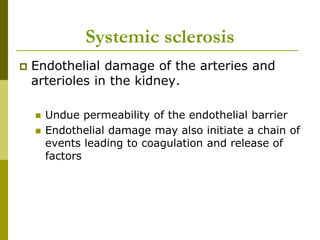
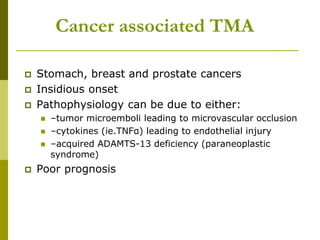
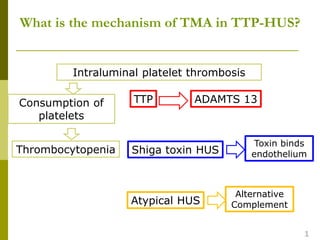
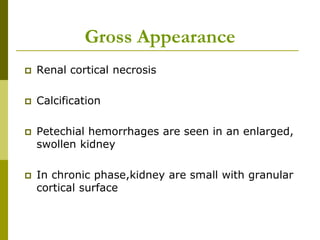
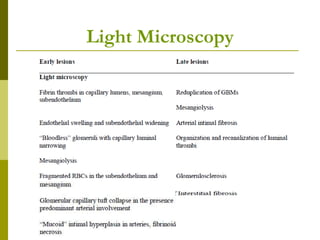
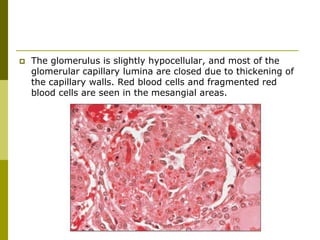
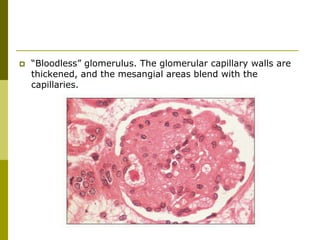
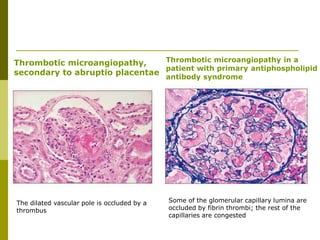
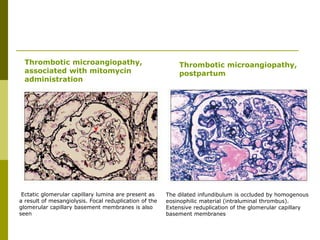
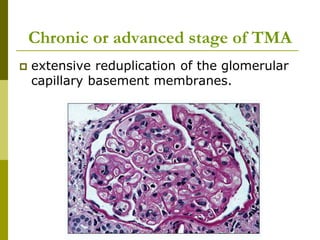
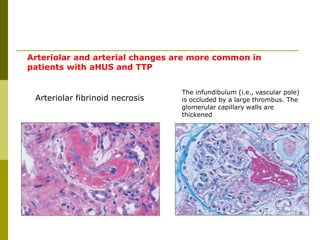
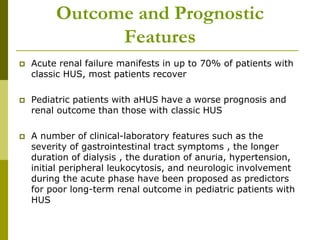
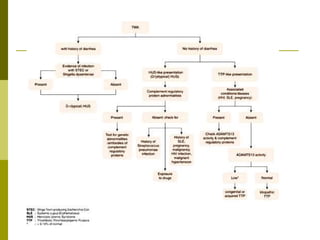
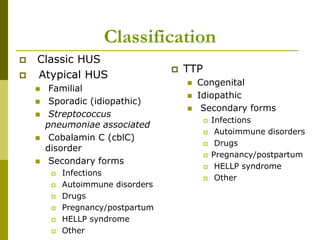
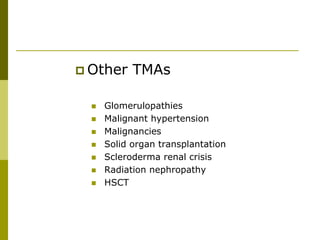
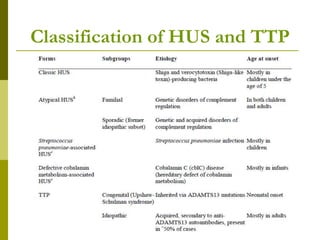
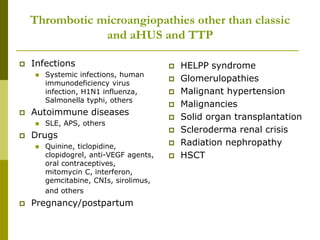
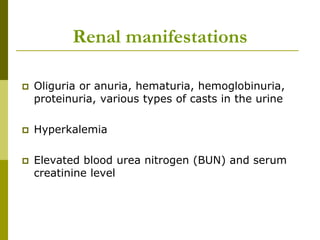
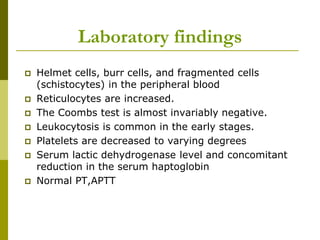
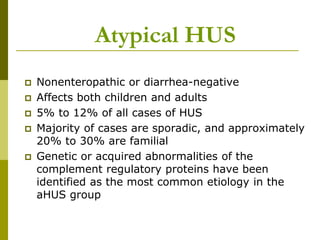
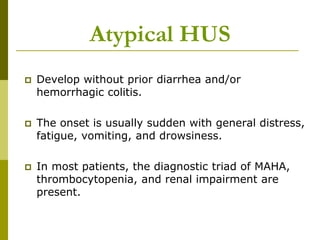
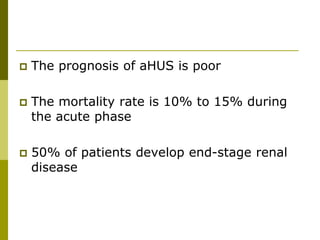
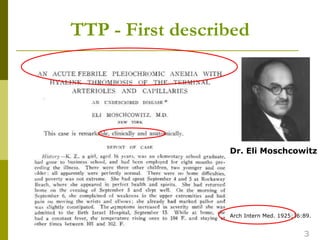
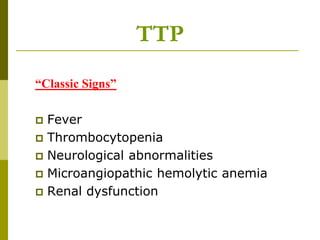
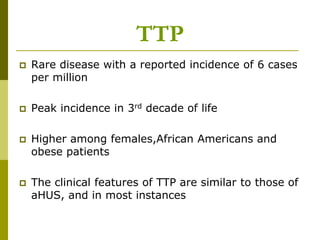
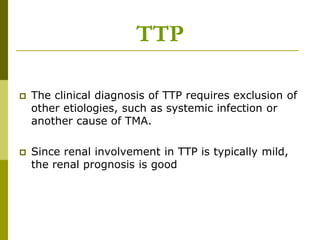
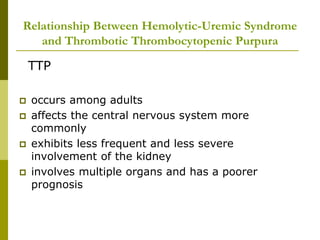
The document discusses thrombotic microangiopathy, which includes classifications such as classic hemolytic uremic syndrome (HUS) and thrombotic thrombocytopenic purpura (TTP), detailing their pathophysiology, clinical presentations, laboratory findings, and prognostic features. It also covers various causes and associated conditions, transmissions, and outcomes, highlighting the differences between classic and atypical HUS and TTP, as well as treatment options. The analysis emphasizes the importance of recognizing the underlying mechanisms and varying prognoses associated with these microangiopathies.
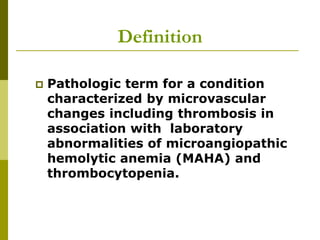
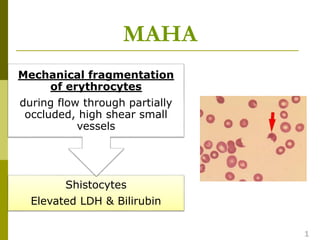
![One underlying fact
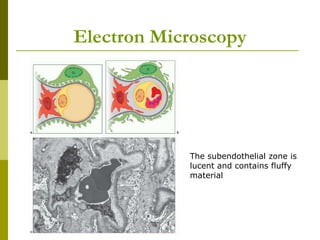
Endothelial damage
[stx,Complement,neuraminidase,drugs]
Exposure of subendoth.surface with Platelet
activation and aggregation
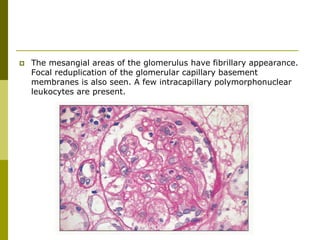
Thrombi and cellular proliferation in glomeruli
and arterioles. Red blood cell hemolysis is
caused by mechanical disruption in traversing
fibrin meshwork of microcirculation](https://image.slidesharecdn.com/thromboticmicroangiopathy-190617152223/85/Thrombotic-microangiopathy-23-320.jpg)