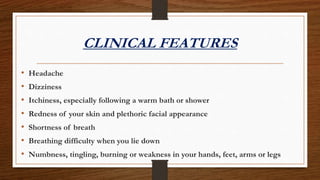
Polycythemia is a blood disorder characterized by excessive production of blood cells, often identified through elevated hemoglobin or hematocrit levels. It can be classified into relative and absolute types, with polycythemia vera being a primary form caused by mutations, particularly in the JAK2 gene. Treatment focuses on reducing red blood cell mass through methods like phlebotomy and medication management to alleviate symptoms and complications.


















![• Ruxolitinib (Jakafi), a JAK1/JAK2 inhibitor, was approved by the FDA in December 2014
for the treatment of patients with polycythemia vera who have had an inadequate response
to or are intolerant of hydroxyurea. Approval was based on data from the phase III
RESPONSE trial. In this trial, patients treated with ruxolitinib demonstrated superior
hematocrit control and reductions in spleen volume compared with best available therapy. A
greater proportion of patients on the ruxolitinib treatment arm achieved complete
hematologic remission (ie, hematocrit control and lowered platelet count and WBC).
Hematologic adverse reactions are prevalent with ruxolitinib (incidence >20%) and include
thrombocytopenia and anemia.[24]
• Ruxolitinib was initially approved in the United States in 2011 for patients with
intermediate- or high-risk myelofibrosis including primary myelofibrosis, post-polycythemia
vera myelofibrosis, and post–essential thrombocythemia myelofibrosis.](https://image.slidesharecdn.com/polycythemia-210530124054/85/Polycythemia-21-320.jpg)
