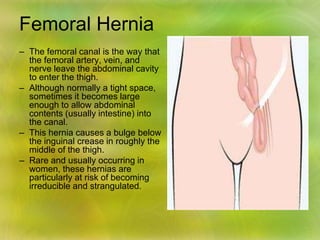
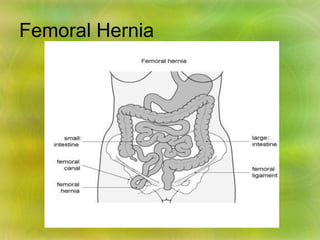
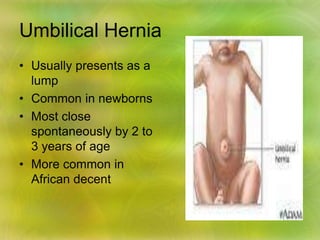
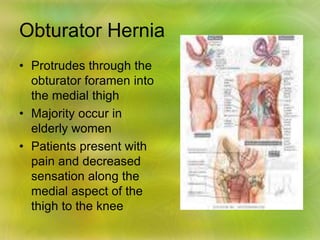
Hernias occur when an internal organ or tissue protrudes through a weakness in the muscle or surrounding wall of the cavity it normally resides in. There are several types of hernias including inguinal, femoral, umbilical, incisional, and others. Risk factors include increased abdominal pressure, obesity, family history, and chronic conditions. Symptoms range from a painless bulge to a painful, swollen protrusion that cannot be pushed back in. Diagnosis involves examination and testing to identify location, contents, and severity. Treatment options depend on severity but typically involve surgical repair to reinforce the weak area, with mesh being commonly used to prevent recurrence.

![Treatment cont.
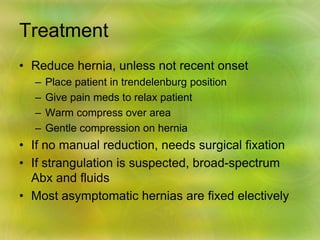
Most abdominal hernias can be surgically repaired.
Uncomplicated hernias are principally repaired
by herniorrhaphy.
a Herniorrhaphy (Hernioplasty) is a surgical
procedure for correcting hernia, which can be
devided into four techniques:
Groups 1 and 2: open "tension" repair:
• in which the edges of the defect are sewn back
together without any reinforcement or
prosthesis. In the Bassini technique, the conjoint
tendon (formed by the distal ends of the
transversus abdominis muscle and the internal
oblique muscle) is approximated to the inguinal
canal and closed. [4]
• Although tension repairs are no longer the
standard of care due to the high rate of
recurrence of the hernia, long recovery period,
and post-operative pain, a few tension repairs
are still in use today.](https://image.slidesharecdn.com/herniabysheetal-210530122621/85/Hernia-24-320.jpg)