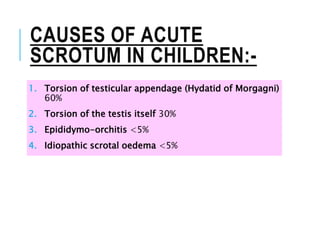
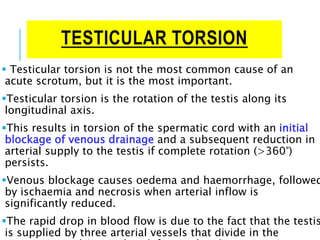
The document discusses acute scrotum, its definition, causes, and management, detailing conditions such as testicular torsion, torsion of appendages, and epididymitis. It emphasizes the importance of urgent exploration in cases where testicular torsion cannot be excluded and outlines the differential diagnosis and clinical examination findings. Additionally, it highlights specific management strategies based on the identified condition, including surgical interventions and conservative treatments.