This document provides information about fetal cardiotocography (CTG), including:
1. CTG can be performed from 28 weeks of gestation as that is when the fetal autonomic nervous system is mature.
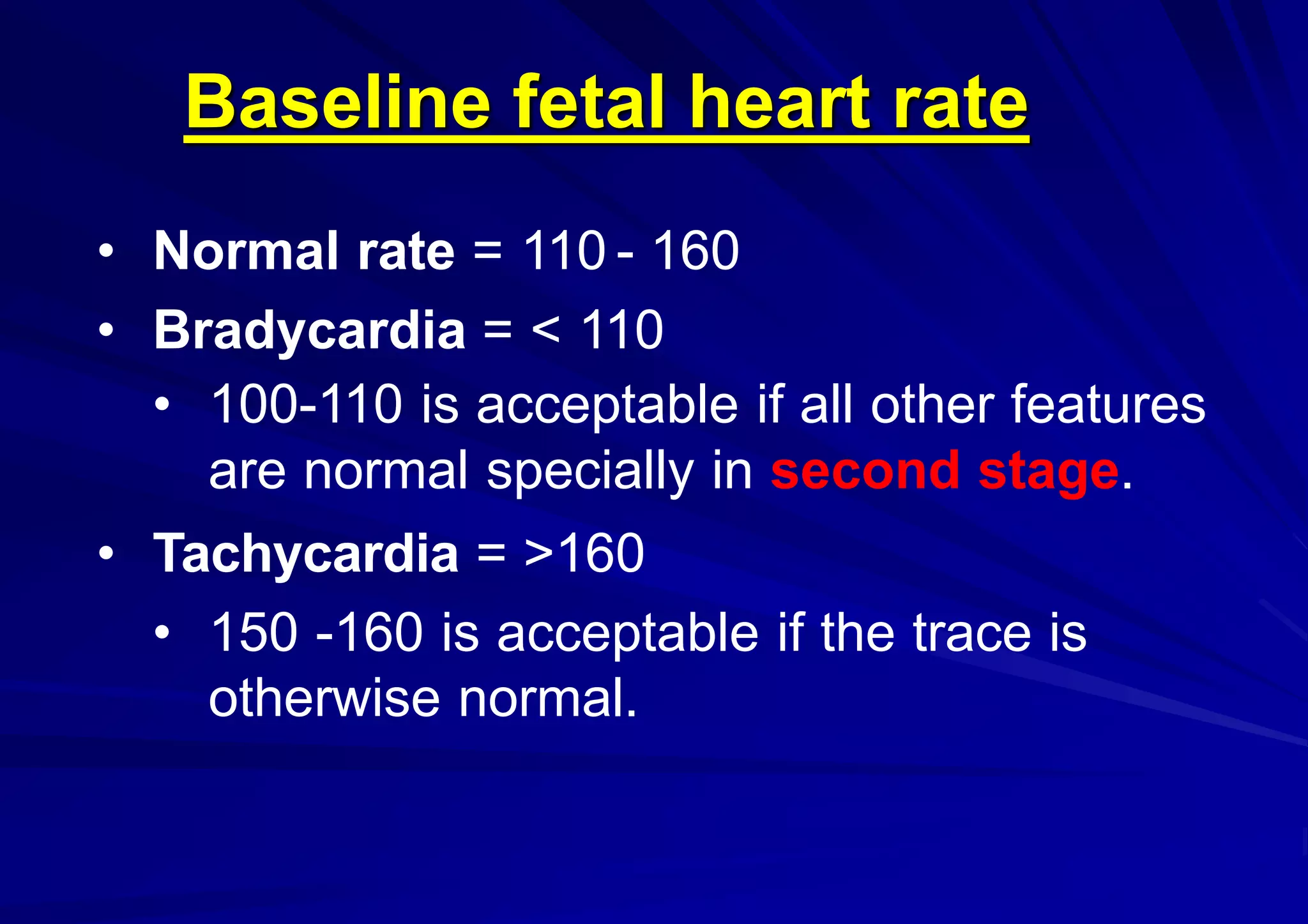
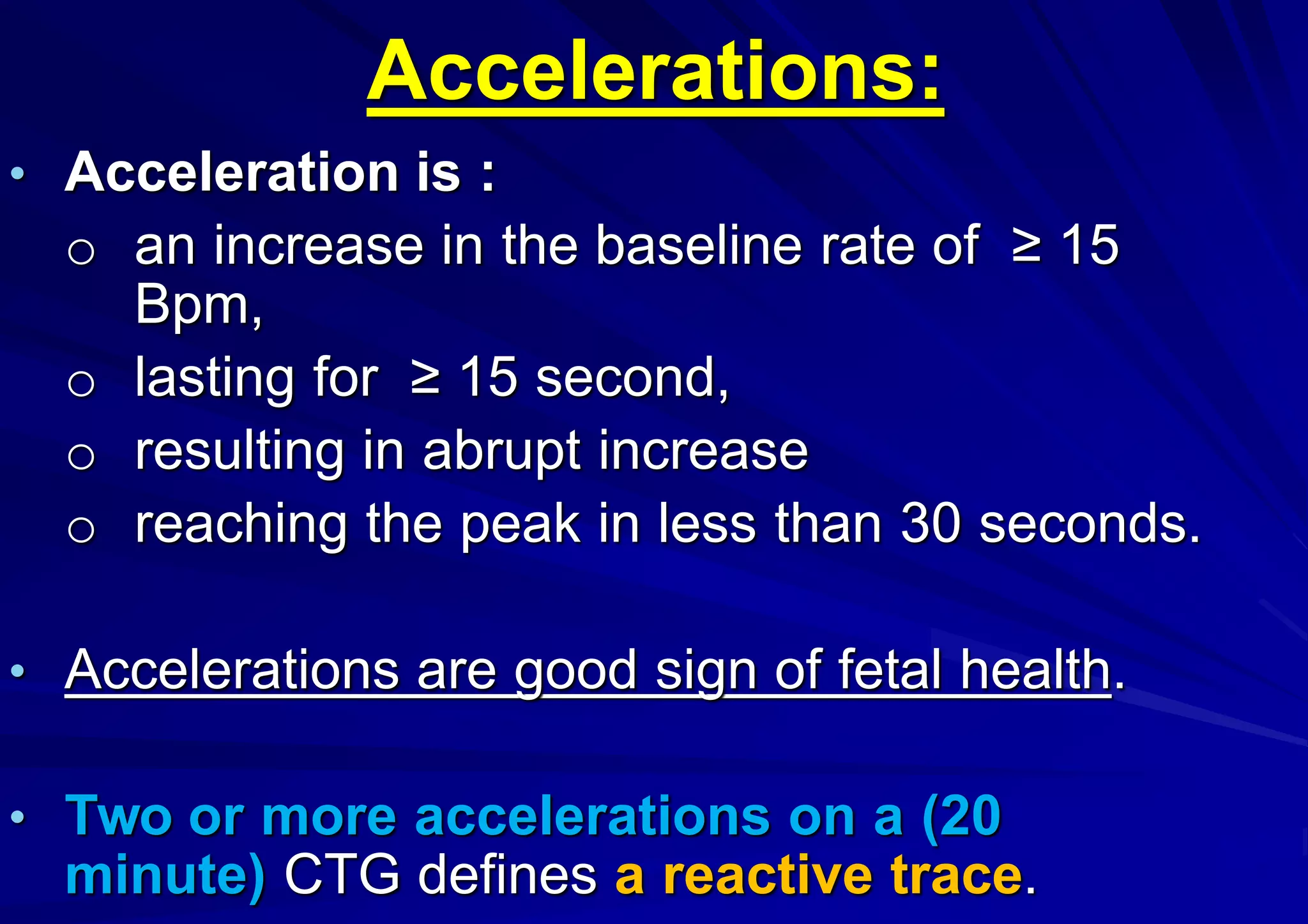
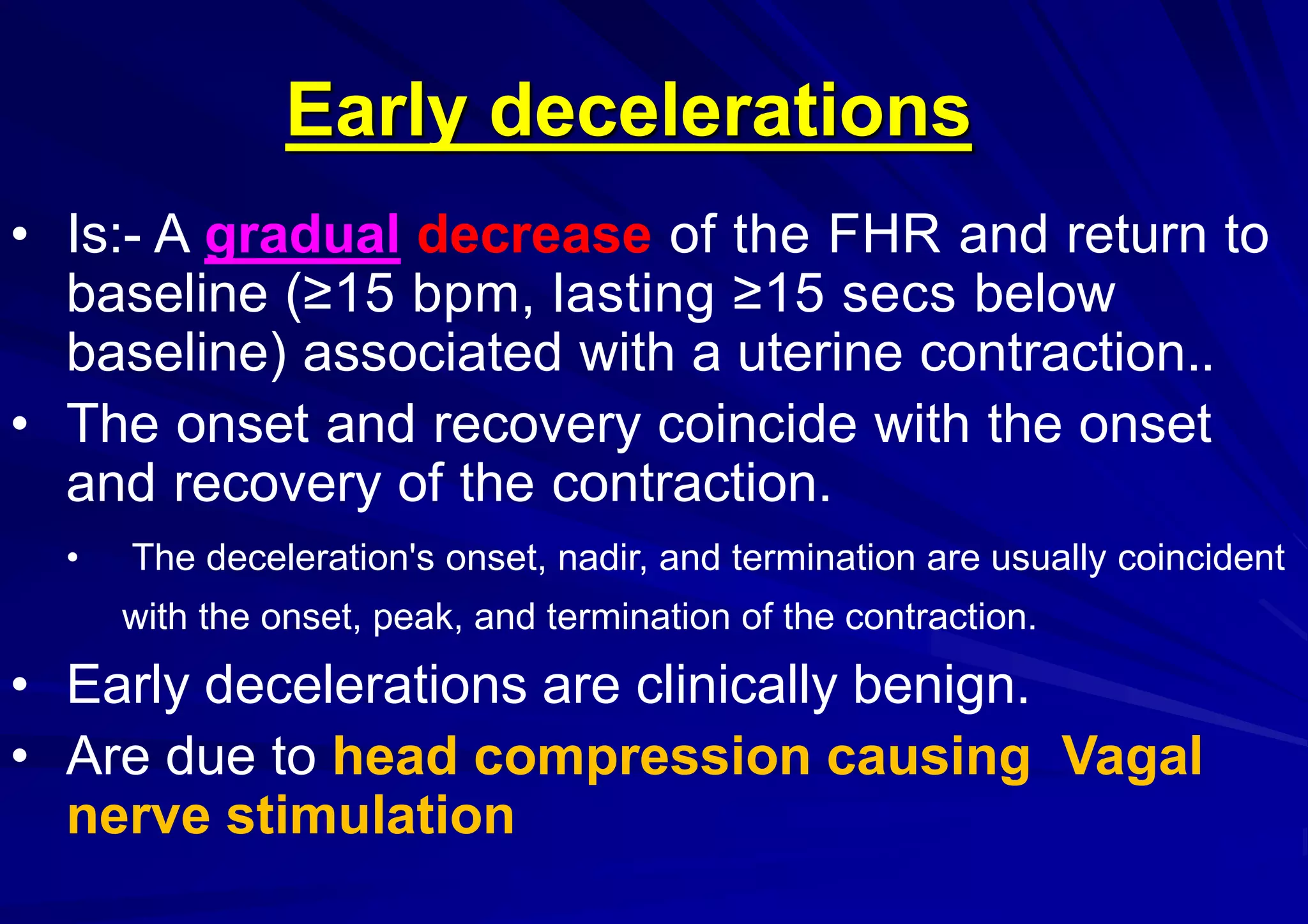
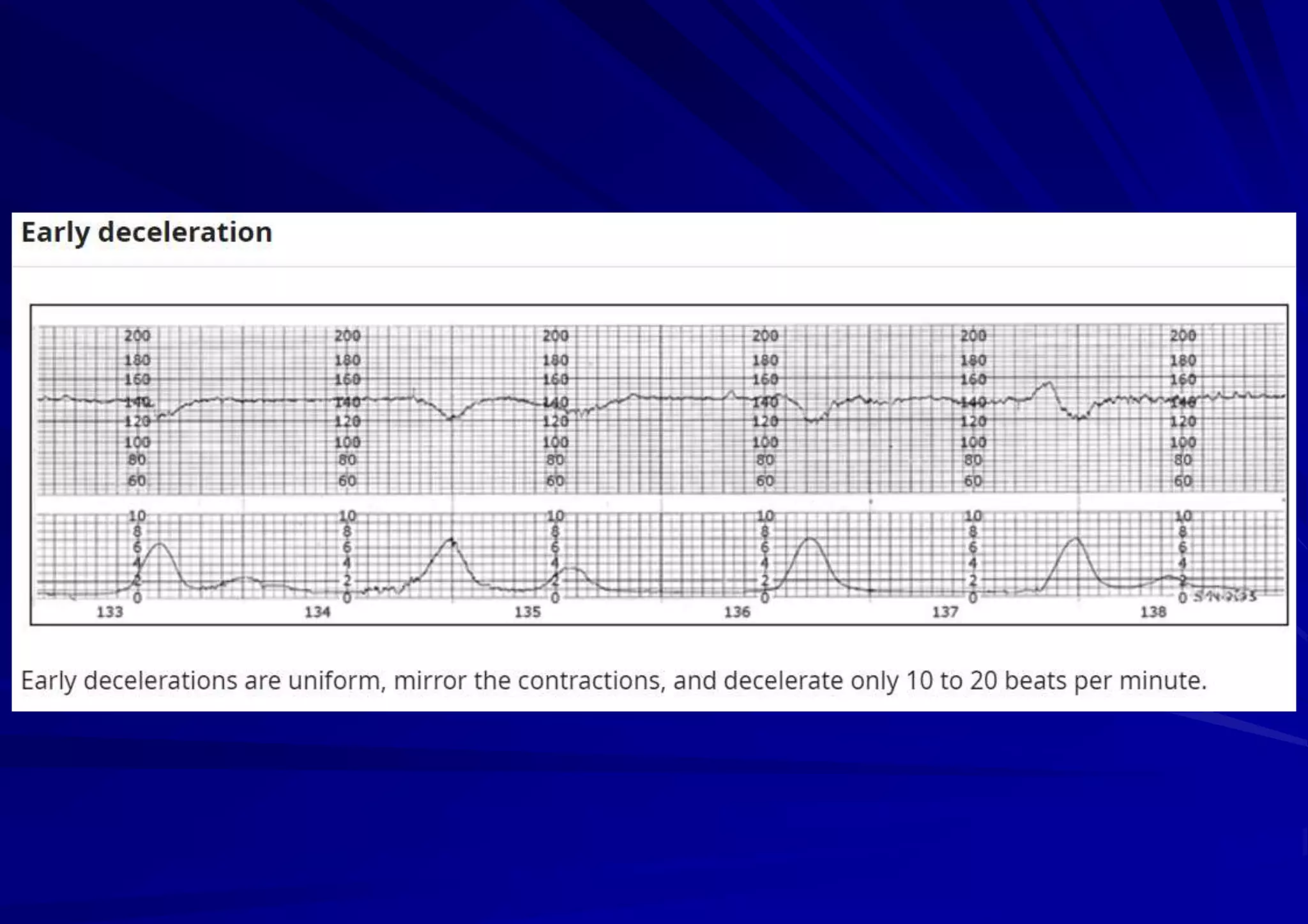
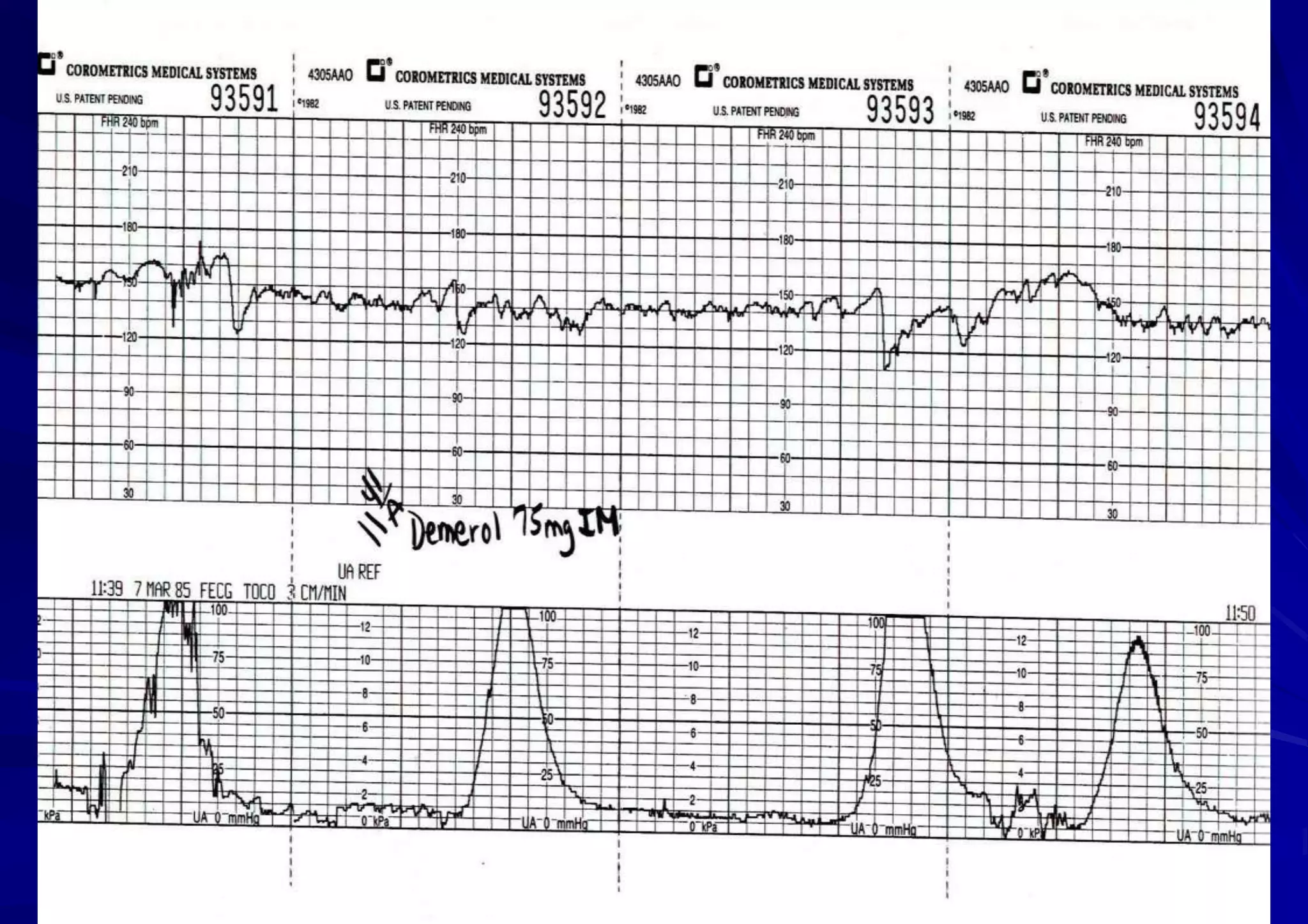
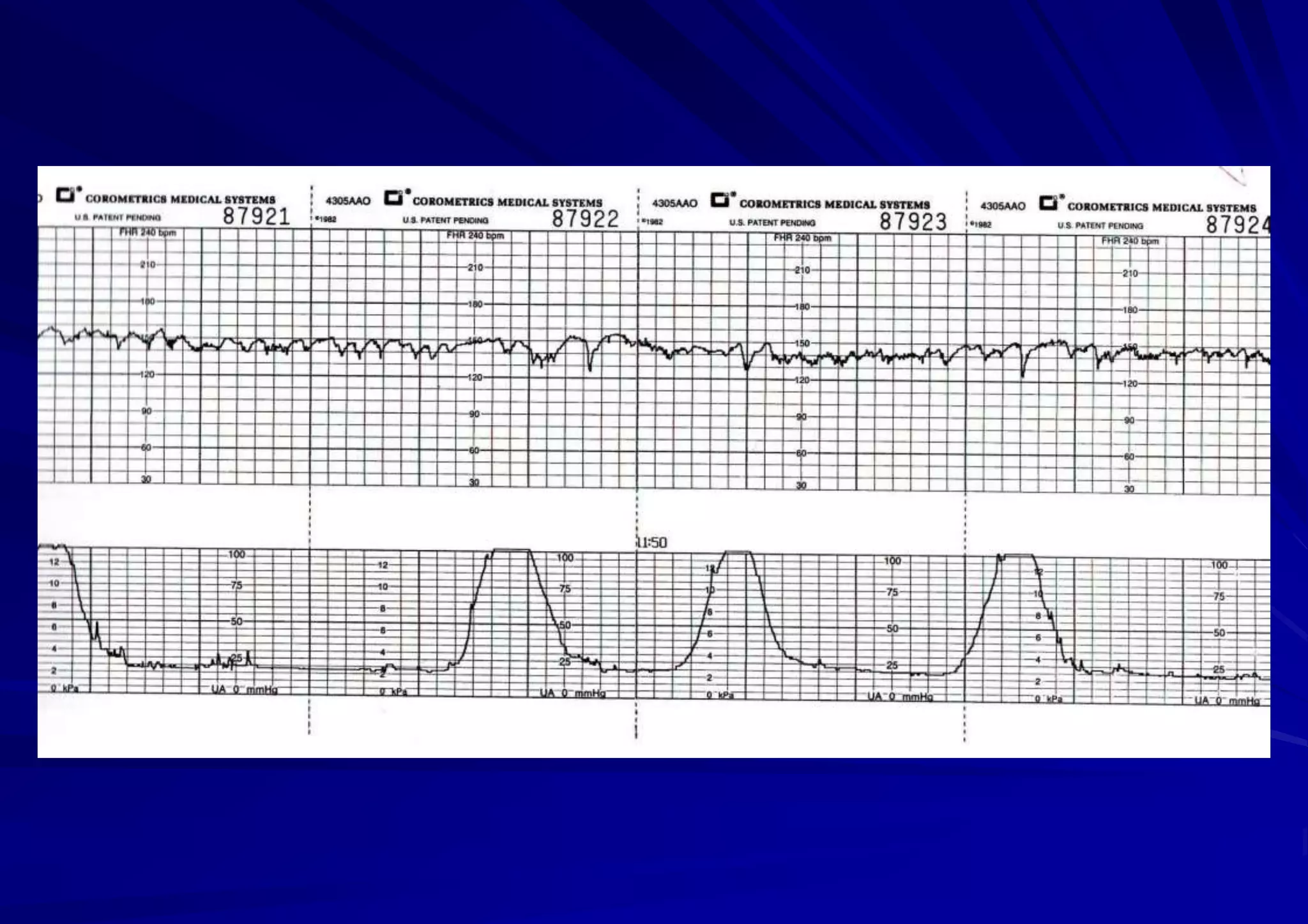
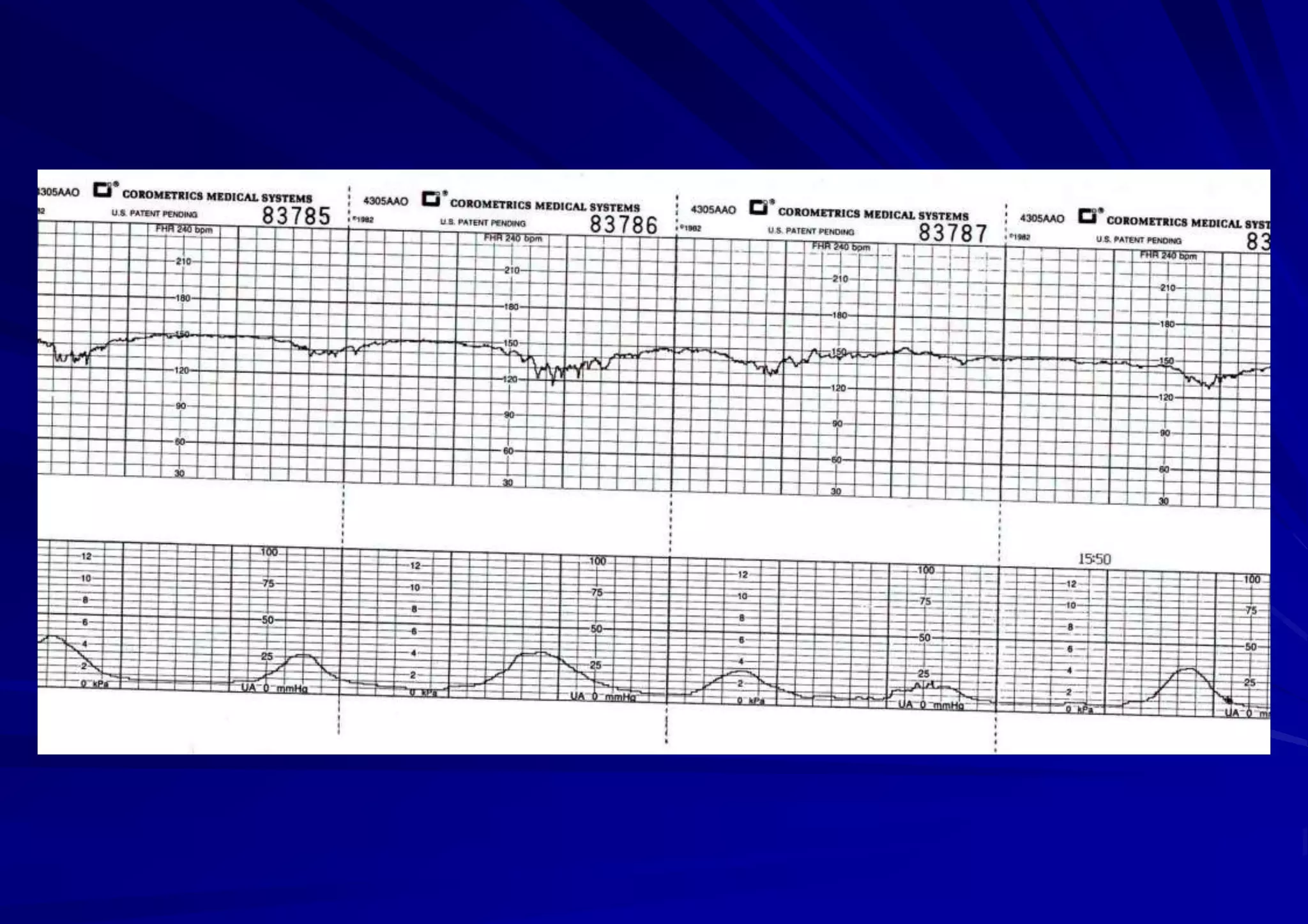
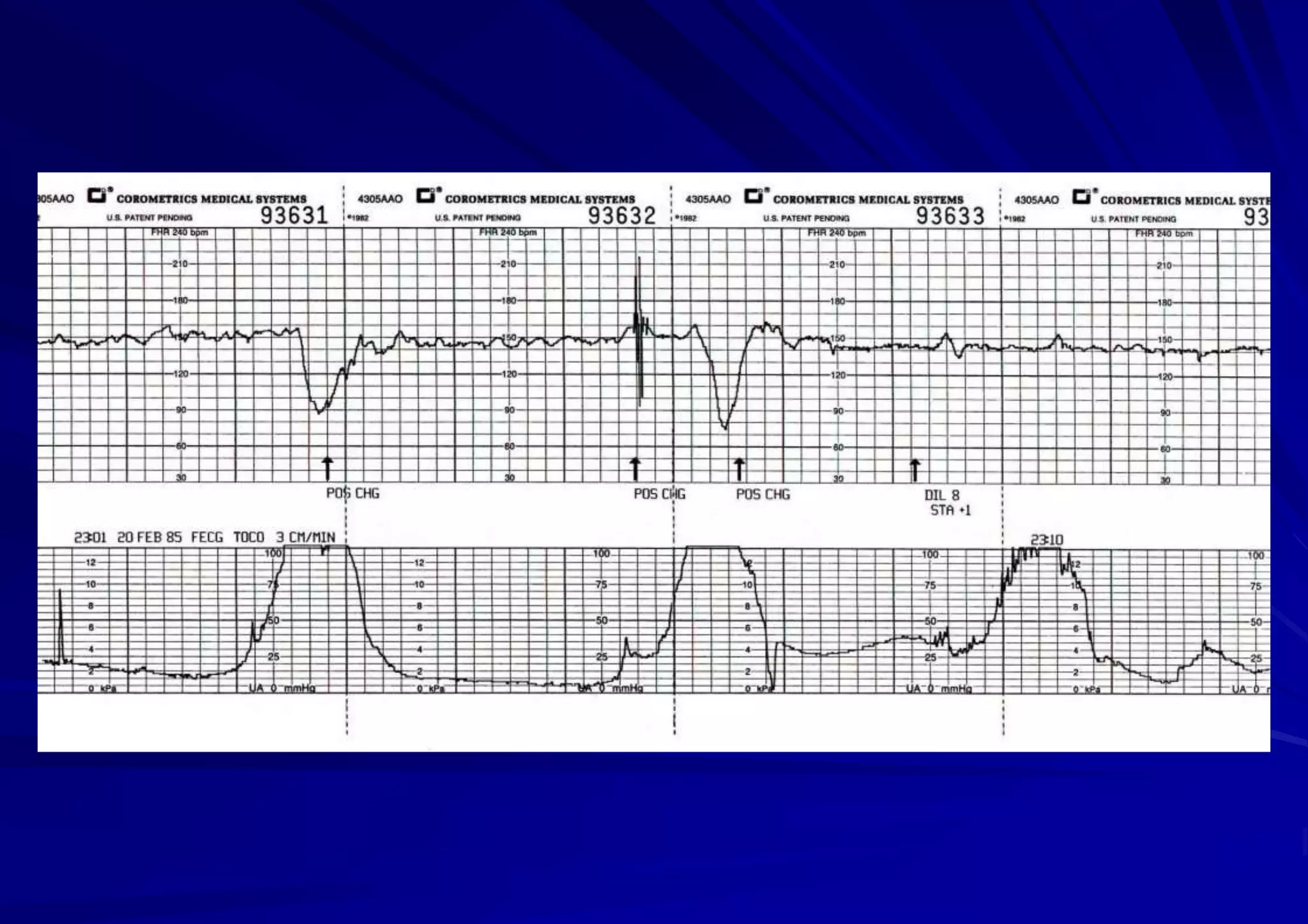
2. Normal CTG findings include a baseline heart rate between 110-160 bpm, variability between 5-25 bpm, and an absence of or early decelerations with at least 2 accelerations in 20 minutes.
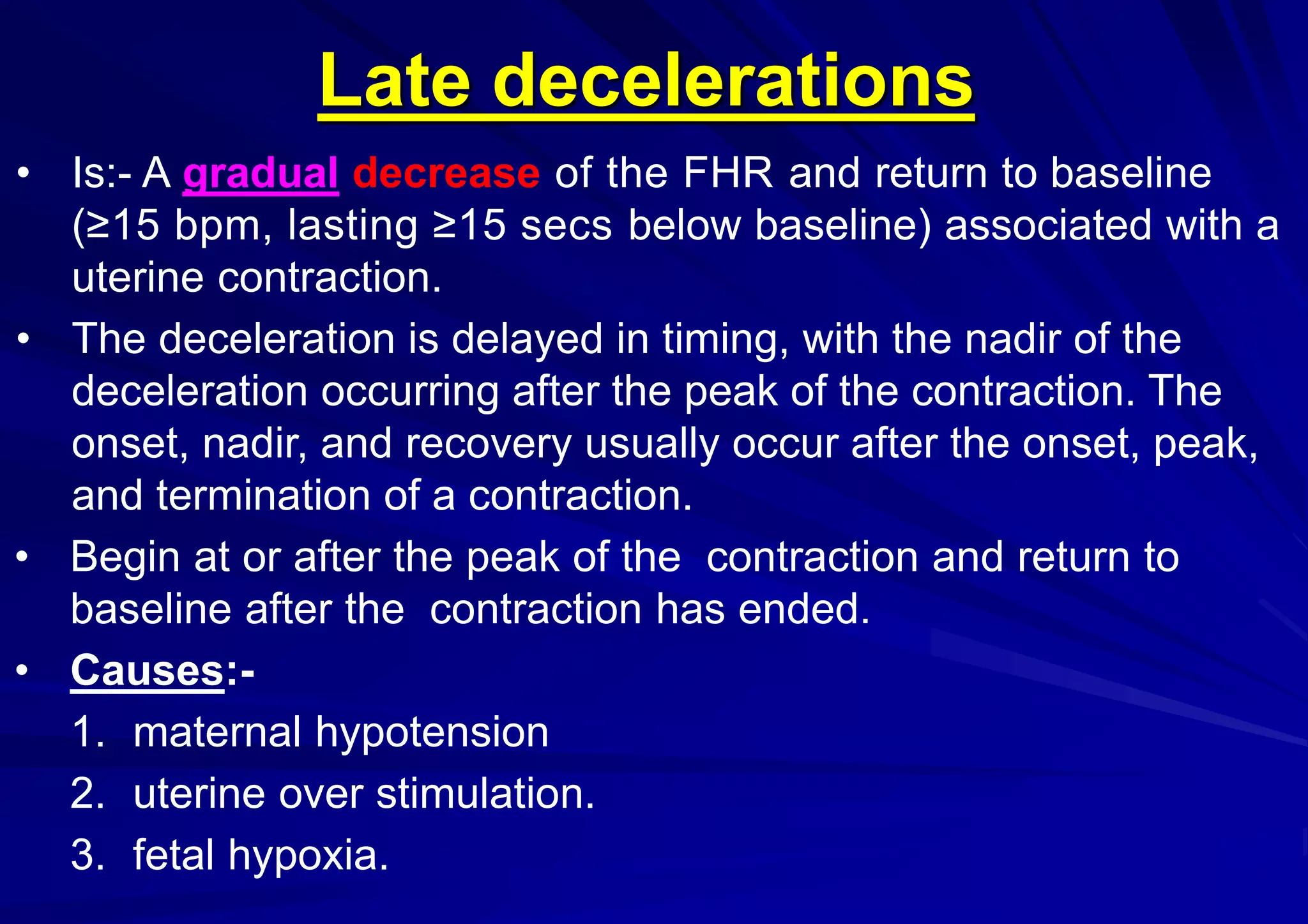
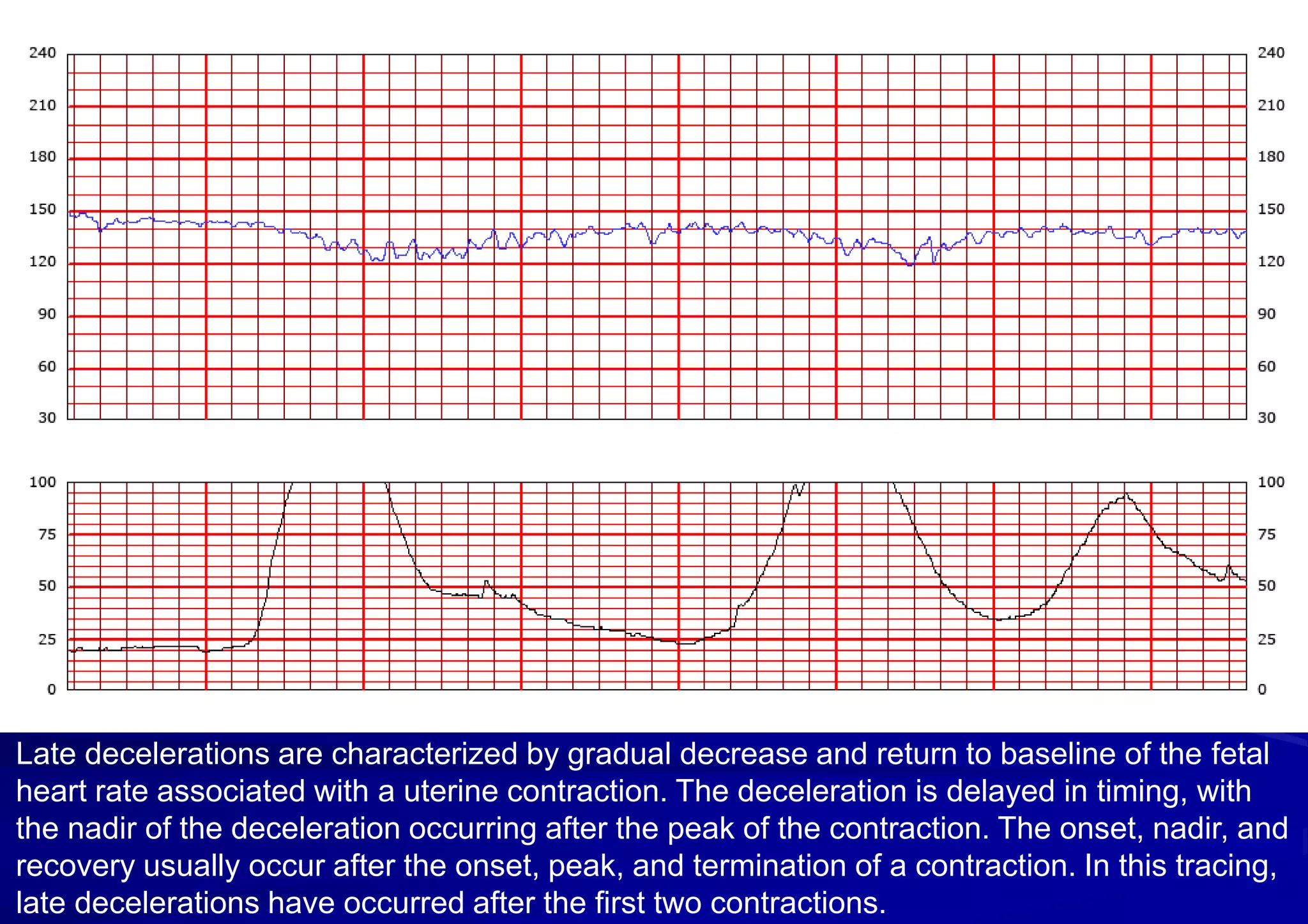
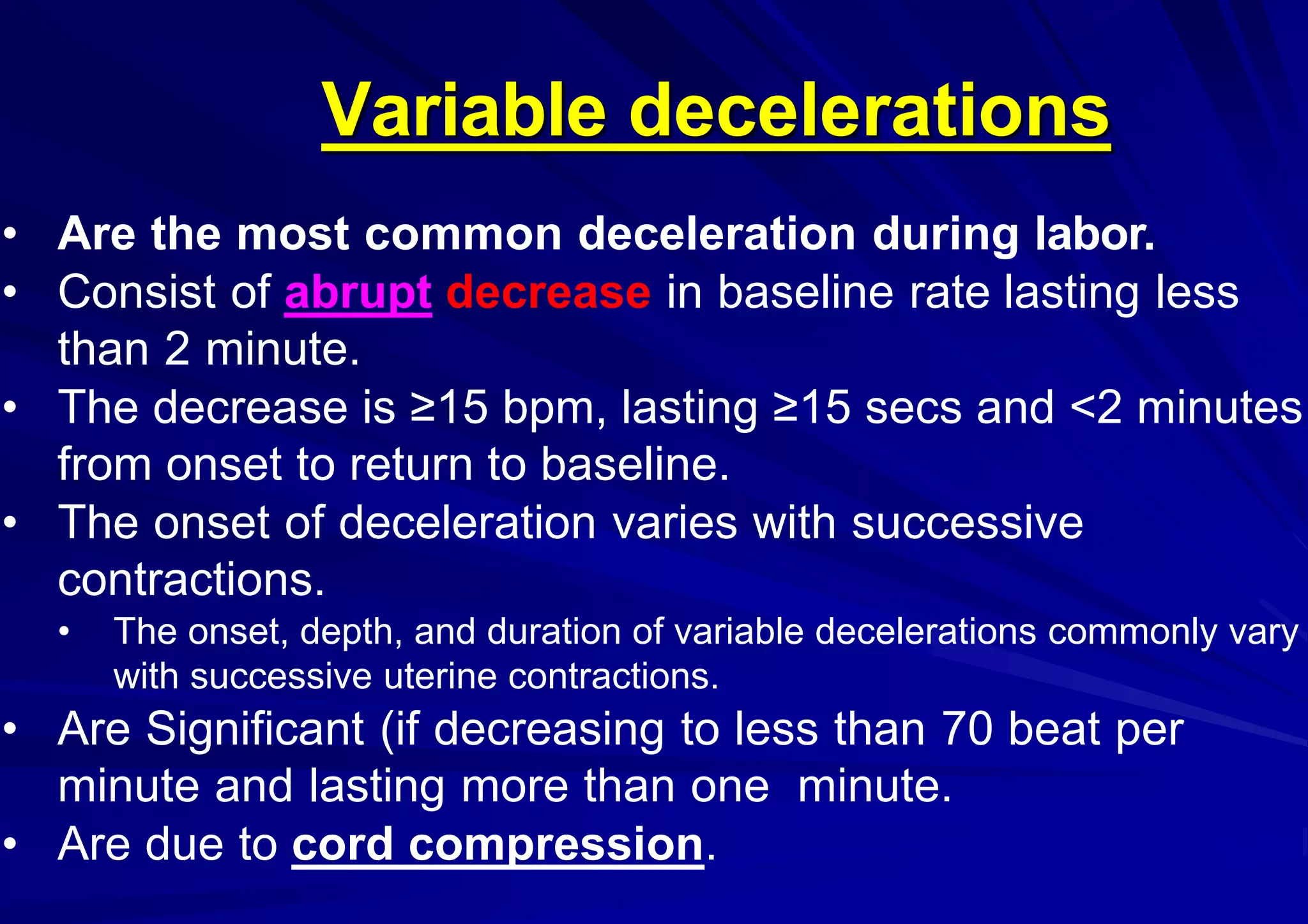
3. Abnormal findings include bradycardia (<110 bpm), tachycardia (>160 bpm), decreased variability (<5 bpm), and late or variable decelerations which can indicate fetal hypoxia or distress.