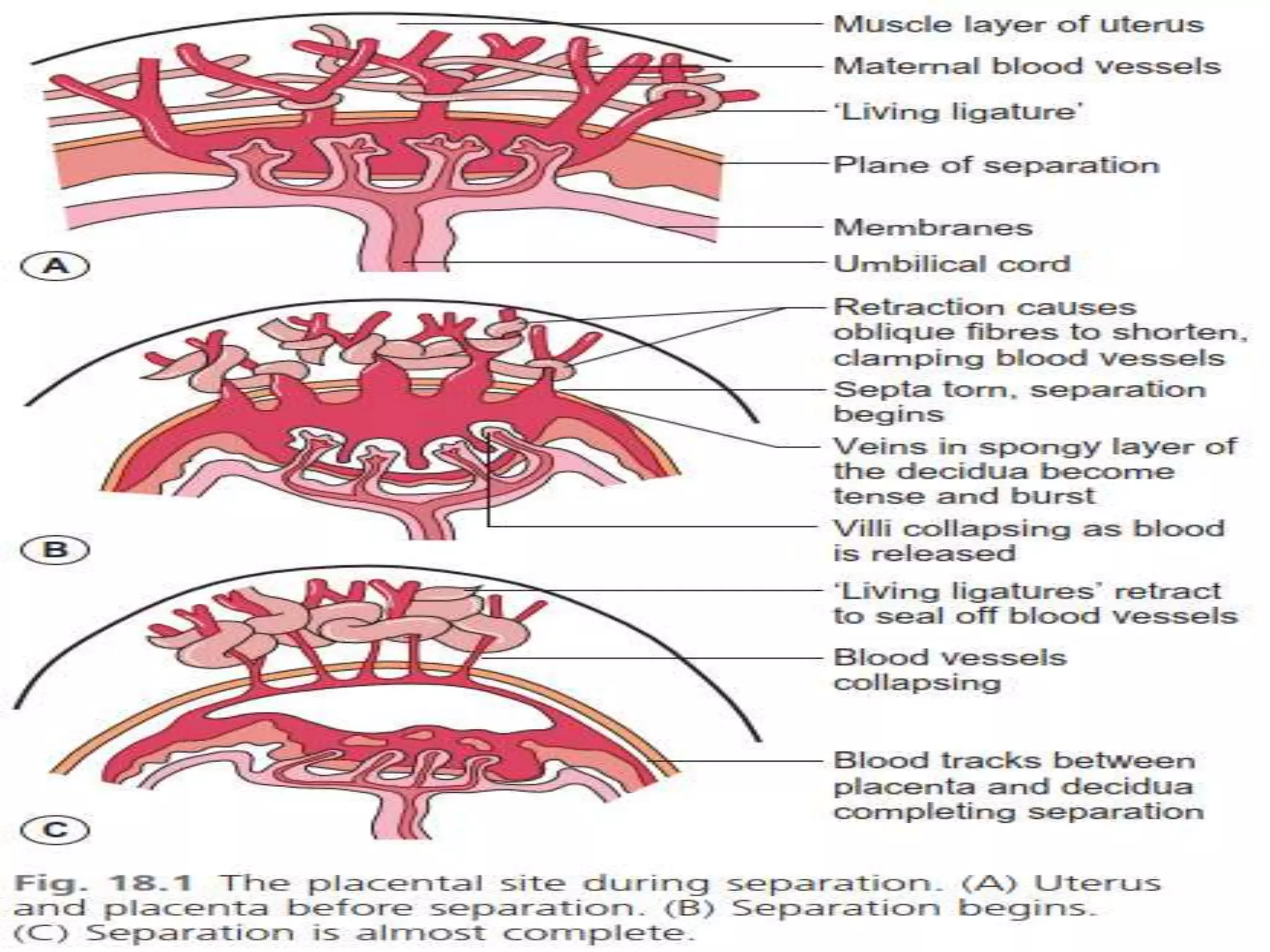
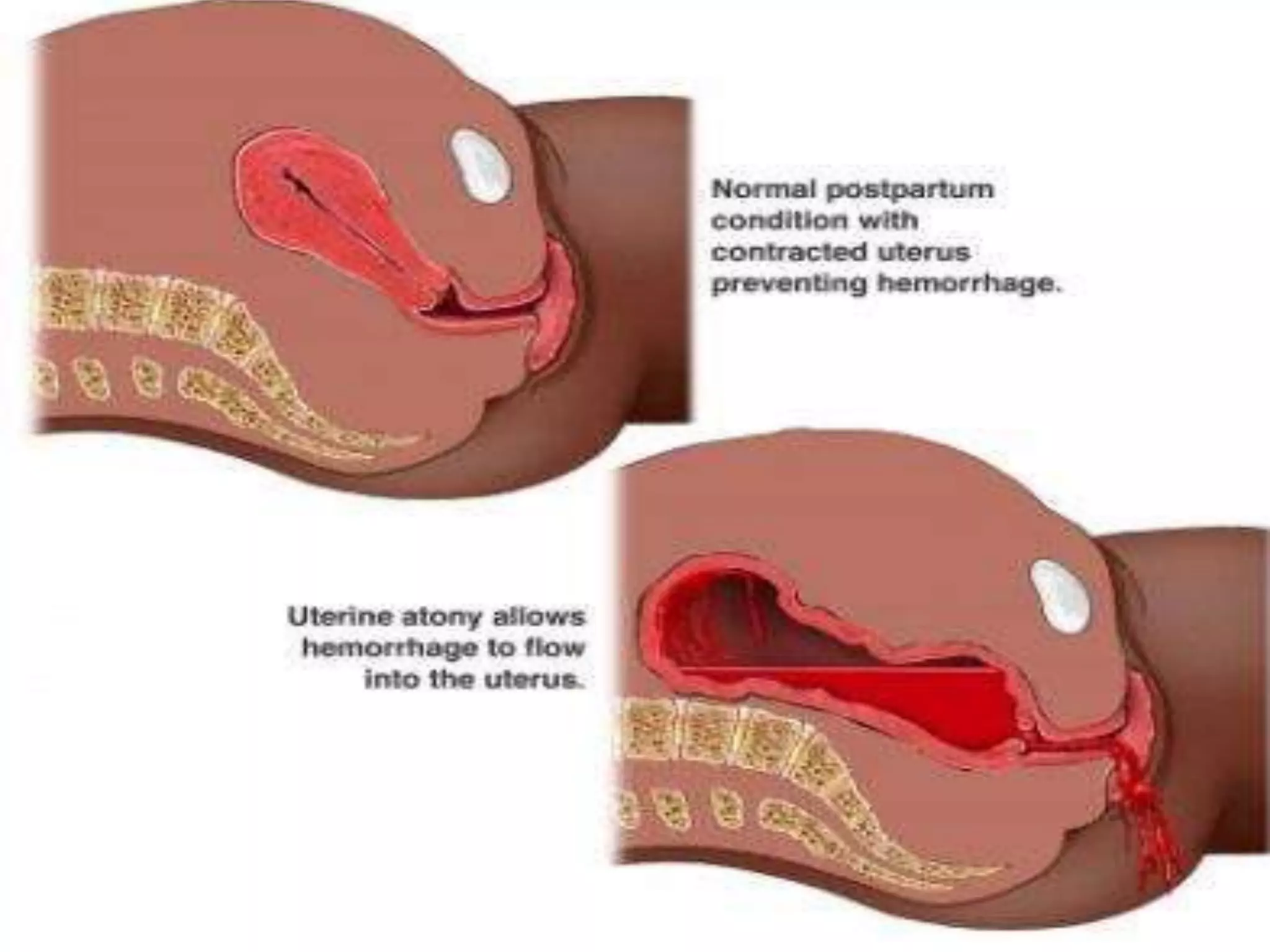
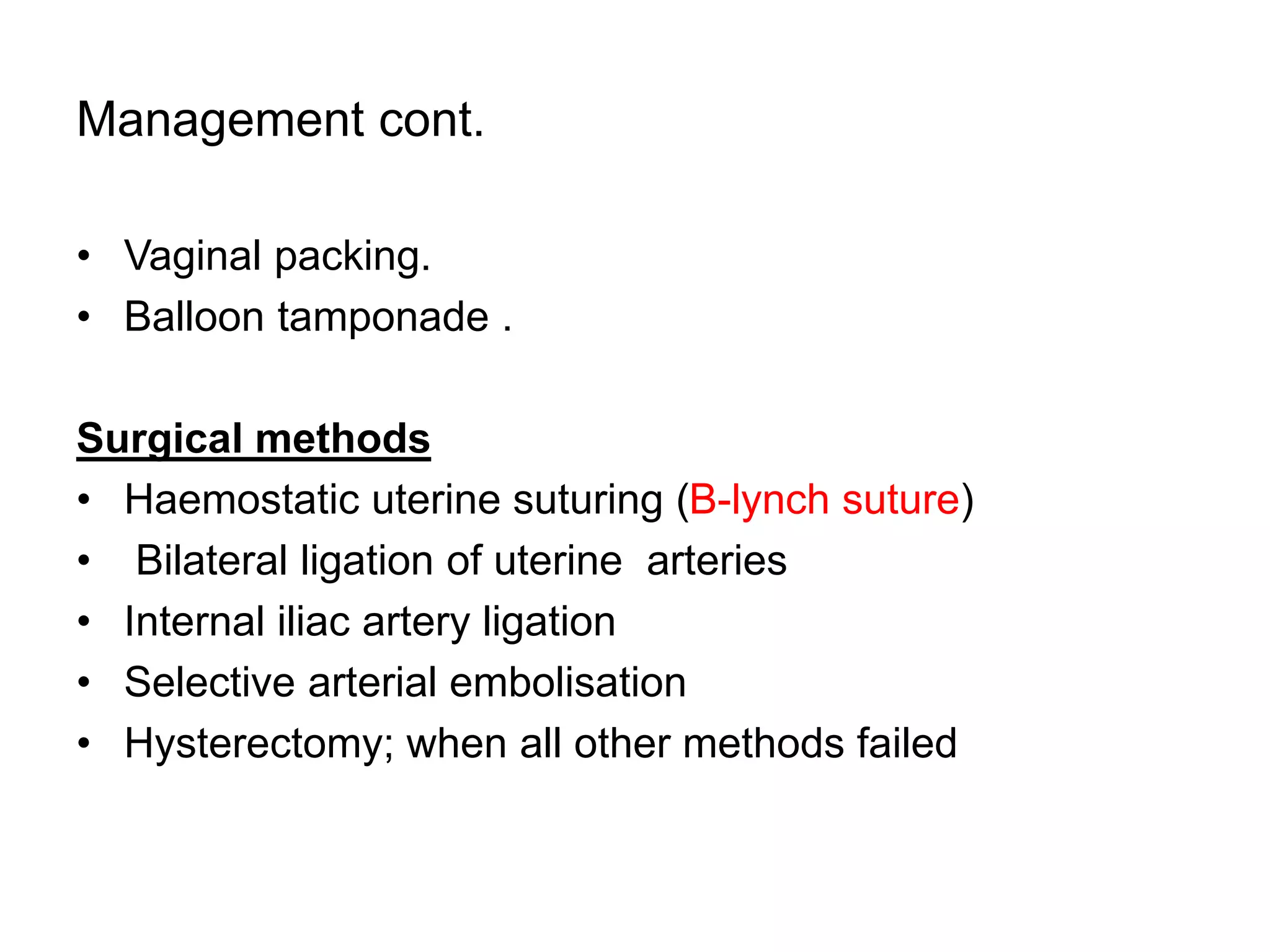
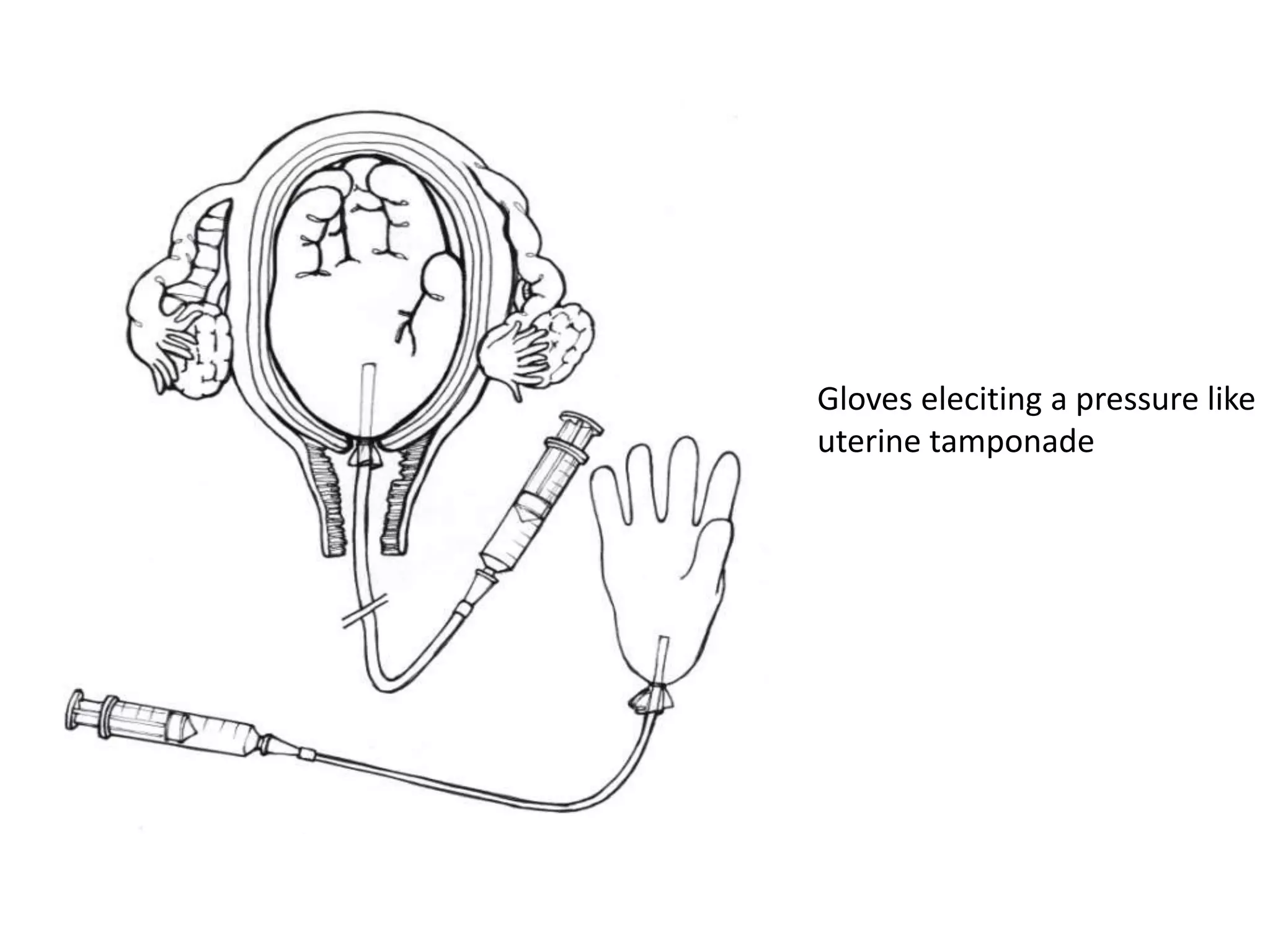
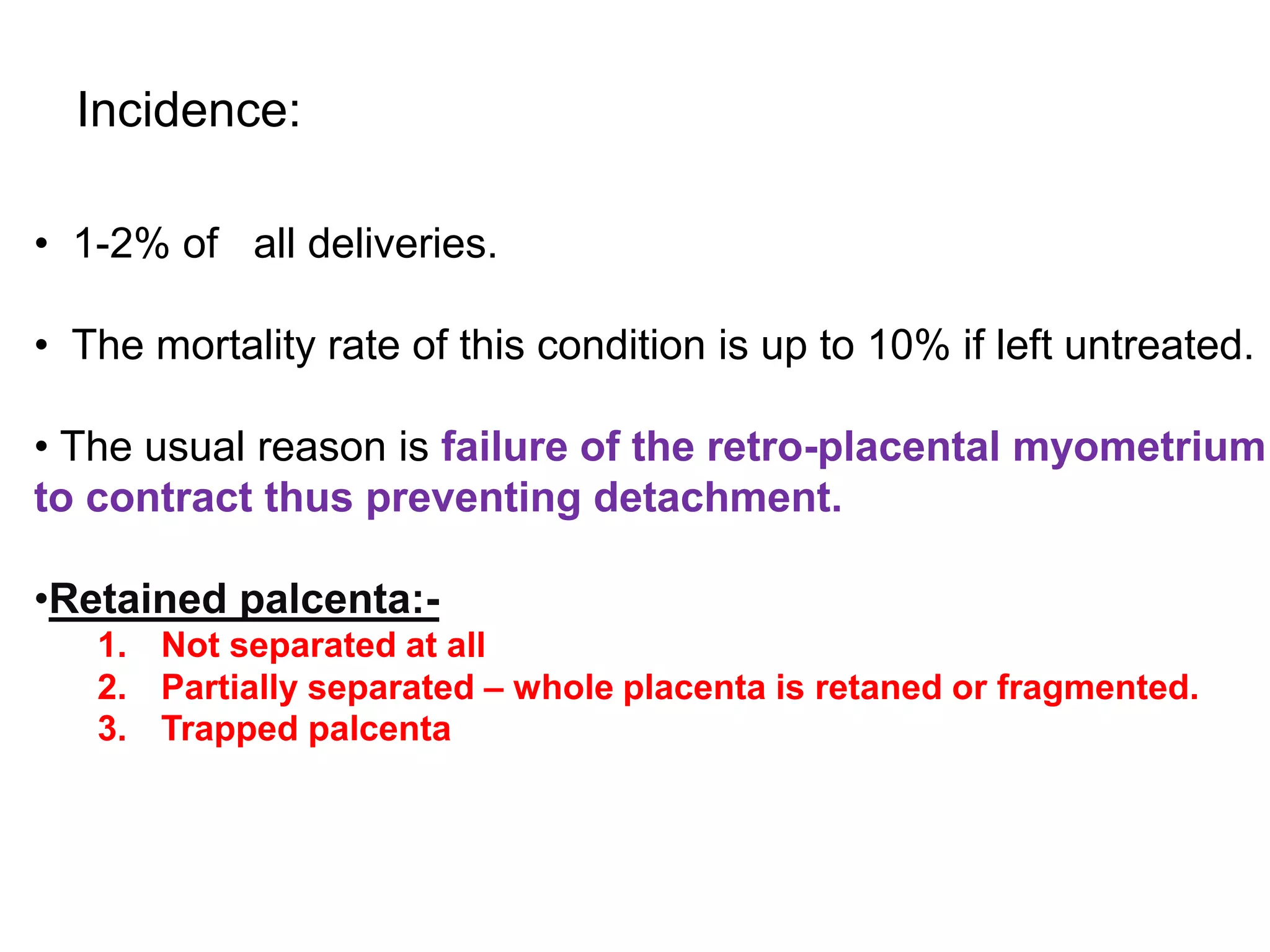
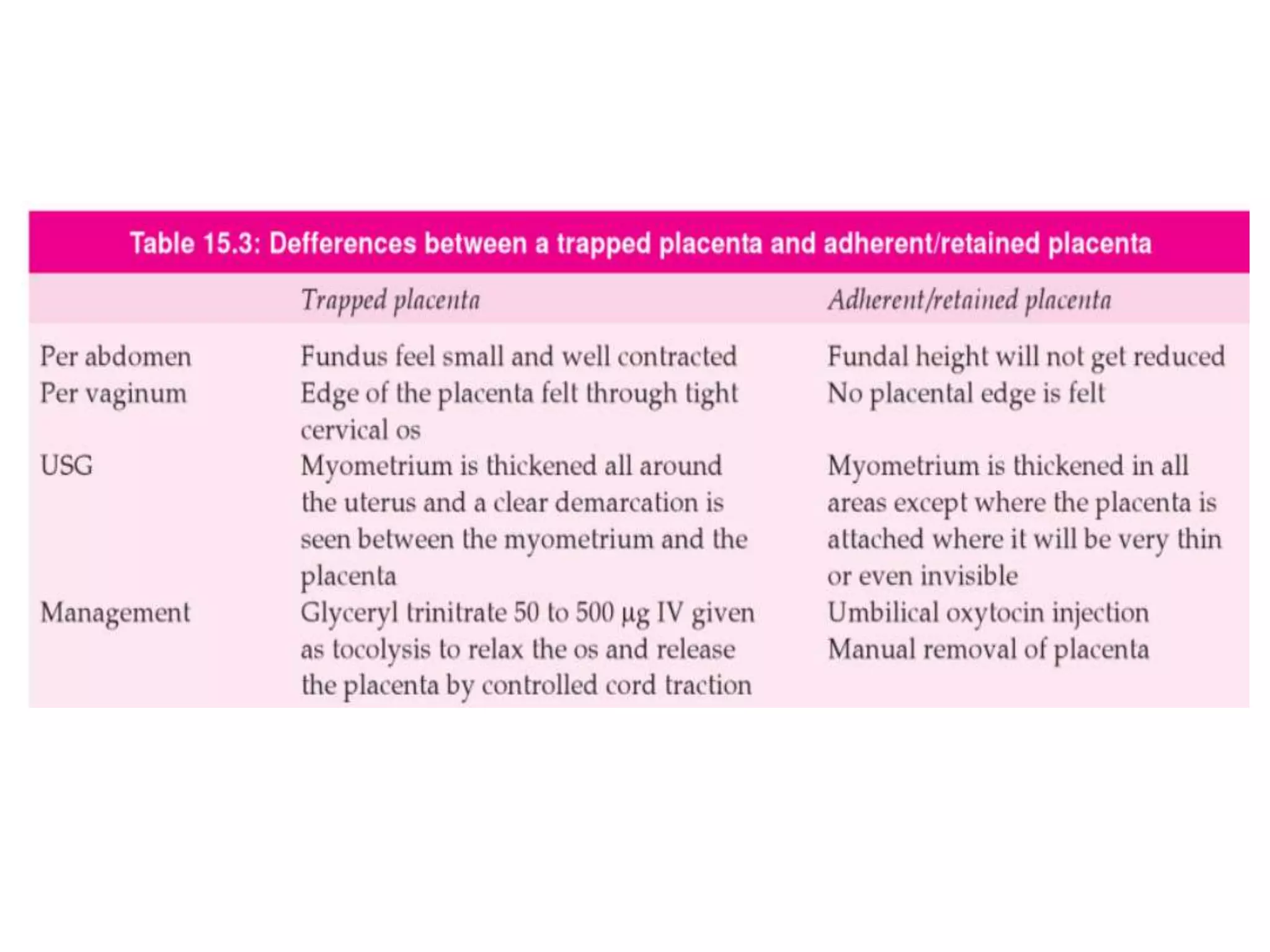
Postpartum hemorrhage (PPH) is excessive bleeding after childbirth, defined as blood loss over 500 ml for vaginal births or 1000 ml for C-sections. The main causes of PPH are uterine atony (failure of the uterus to contract), retained placenta, and trauma to the genital tract. Management involves bimanual uterine massage, uterotonic drugs, vaginal packing, balloon tamponade, and in severe cases surgical interventions like B-Lynch sutures or hysterectomy.