This document provides information on evaluating and diagnosing causes of testicular pain. Key points covered include:
- Taking a history to identify characteristics of the pain, trauma history, changes in testicle size, sexual history, urinary symptoms, and associated abdominal pain.
- Performing a focused exam including inspection, palpation, checking the cremasteric reflex and Phren's sign.
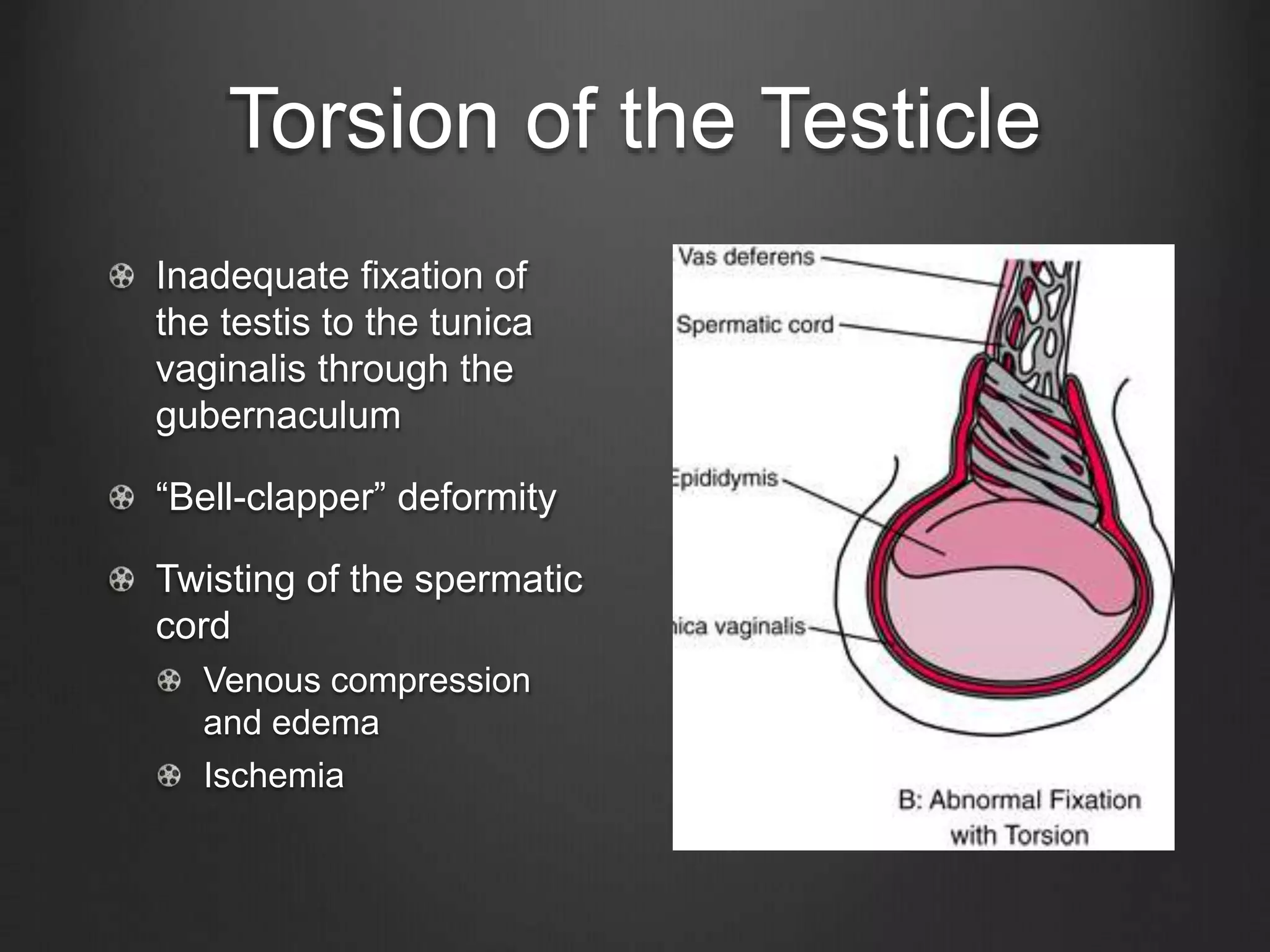
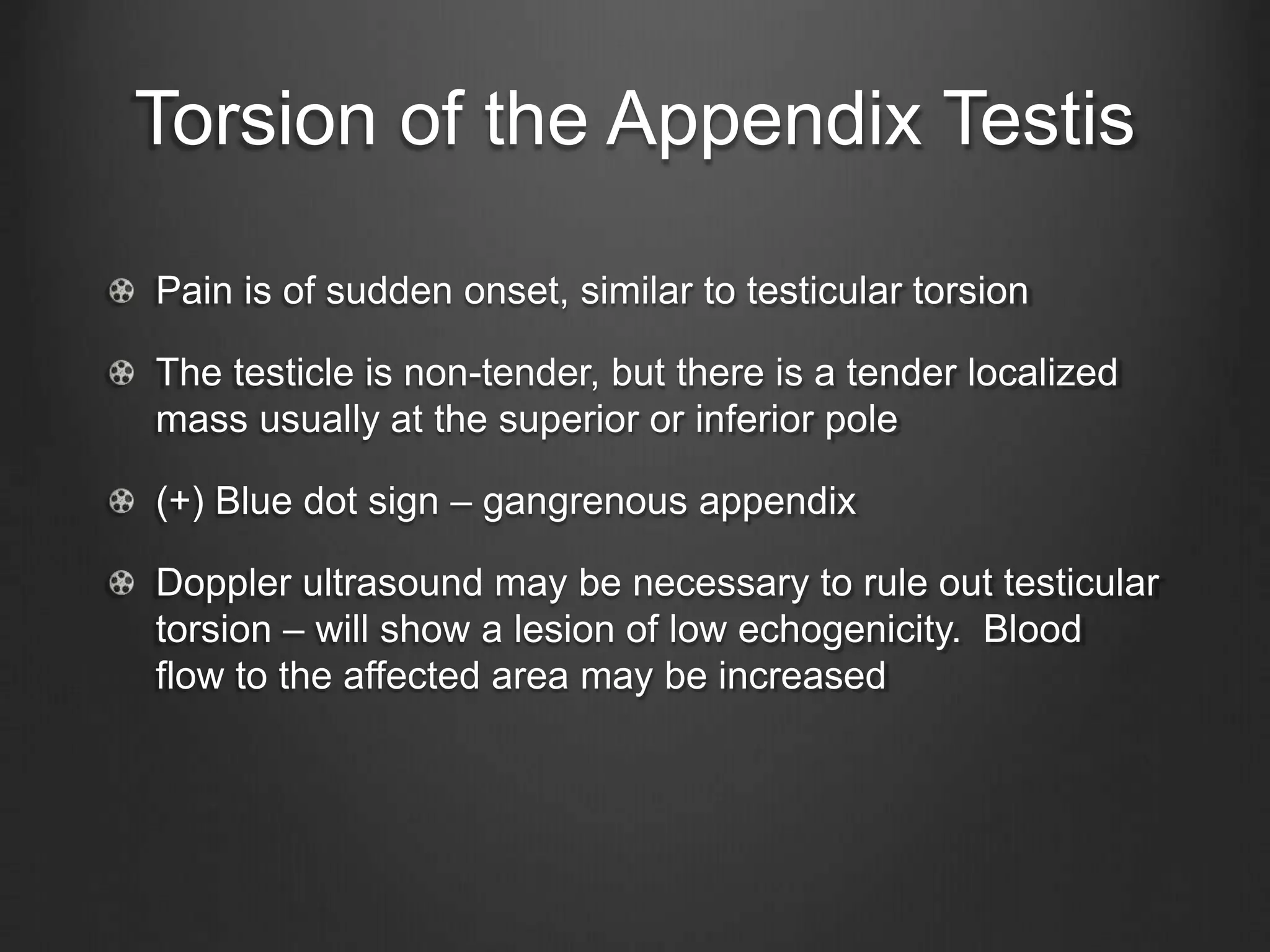
- Common differentials to consider include testicular torsion, torsion of the appendix testis, and epididymitis. Additional tests like ultrasound may help distinguish between causes.
- Management depends on the diagnosis but may include pain medication, antibiotics, manual detorsion in the ER, or surgical correction for torsion






















![Epididymitis
ADMSSION CRITERIA CHILDREN SEXUALLY ACTIVE
Doubt diagnosis
(?Torsion)
(+) Leukocytes in urine
Empiric antibiotics –
Bactrim*/Keflex*
Ceftriaxone x 1 +
Doxycycline x 10
days
Severe pain Ofloxacin
Immunocompromised (-) Leukocytes in urine
Supportive treatment
[NON-BACTERIAL]
Levofloxacin
Unreliable patient
Non-compliance
• It is equally important to treat sexual partners if an STD is the likely
cause.
• Supportive therapy: Scrotal support, bed rest and NSAIDS](https://image.slidesharecdn.com/testicularpain-er-171028151725/75/Testicular-pain-in-emergency-25-2048.jpg)

