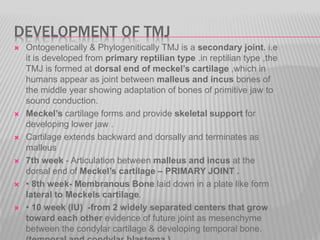
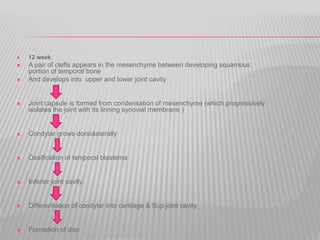
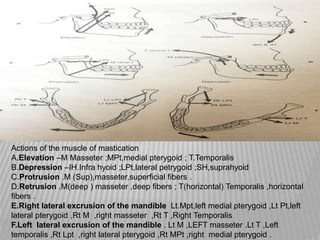
The document provides an overview of the temporomandibular joint (TMJ), including its anatomy, components, development, function, and age-related changes. Key points include:
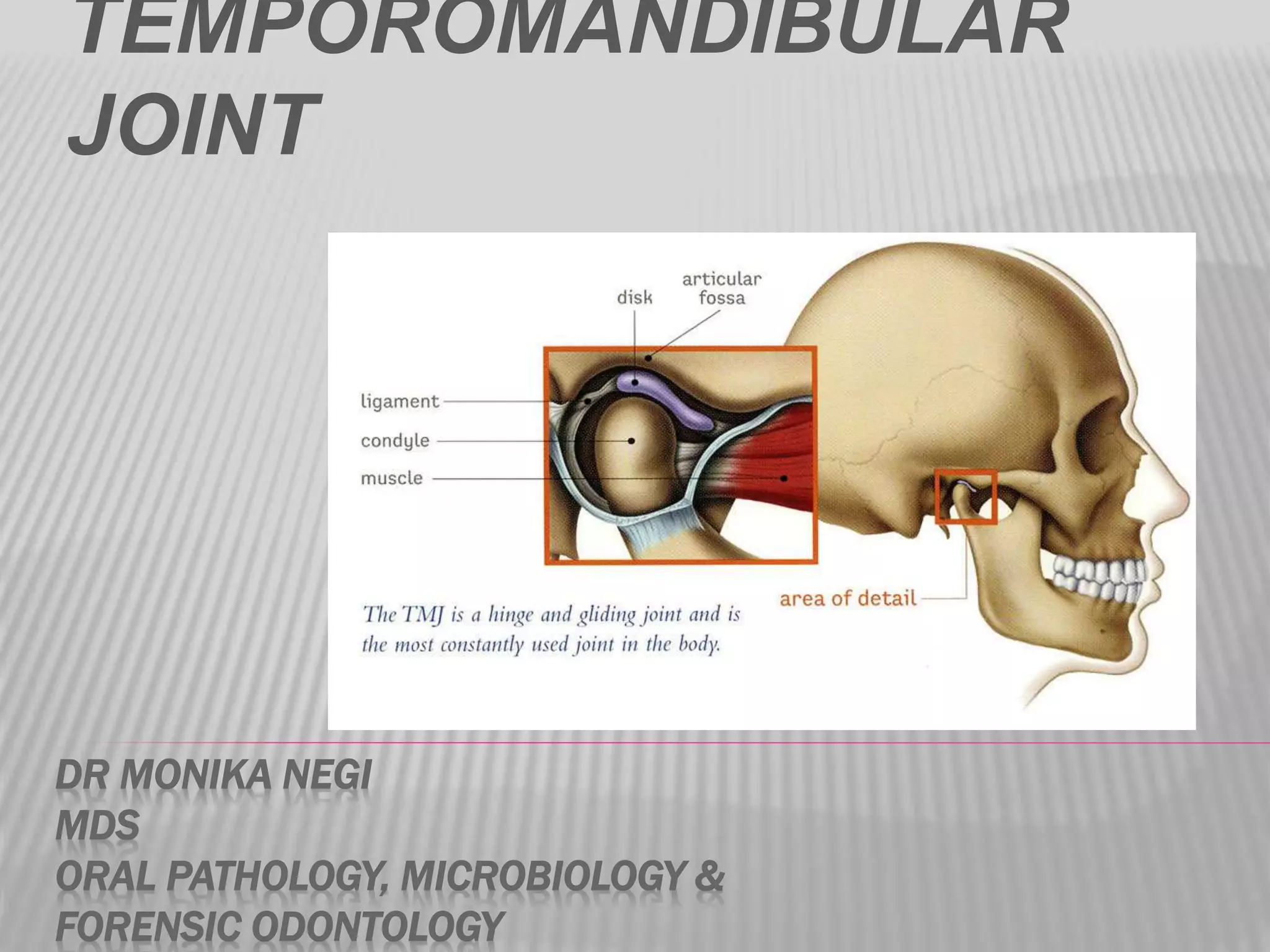
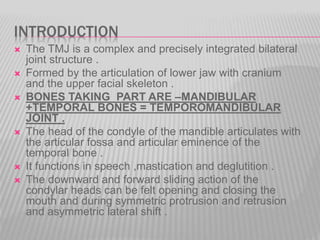
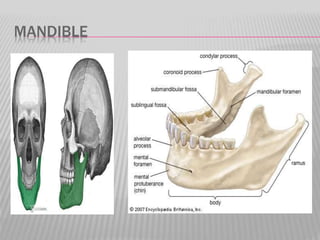
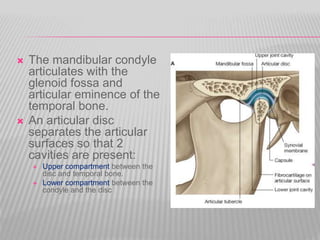
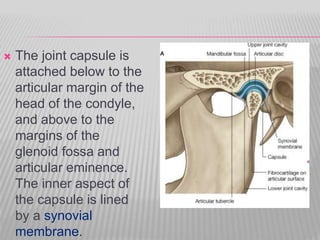
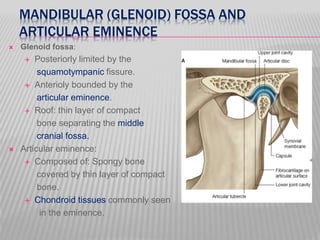
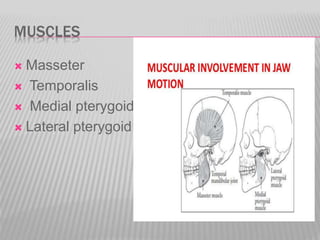
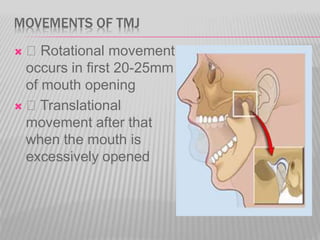
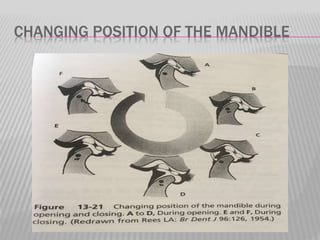
- The TMJ is a synovial joint that permits hinge and gliding movements of the mandible and involves the condyle of the mandible articulating with the temporal bone.
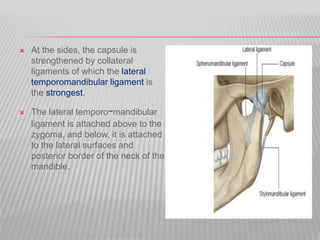
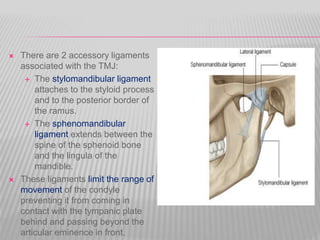
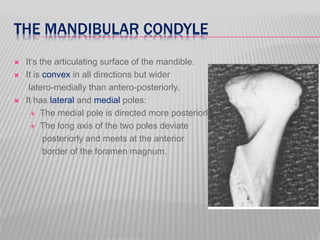
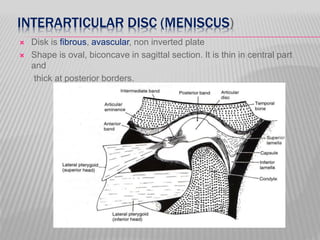
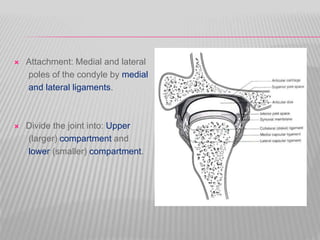
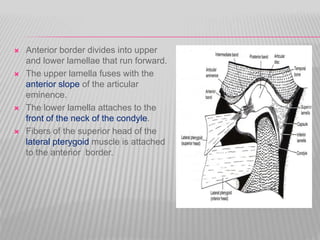
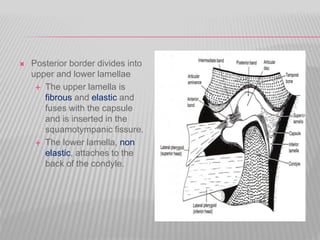
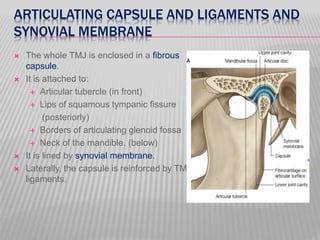
- Its main components are the mandibular condyle, glenoid fossa, articular disc, articular capsule, synovial membrane, and ligaments.
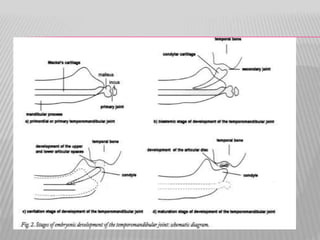
- It develops from Meckel's cartilage and functions in speech, mastication, and deglutition.
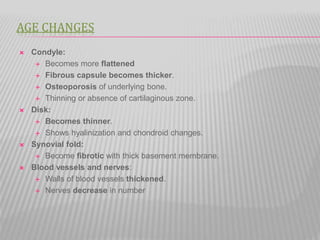
- Age-related changes include fl