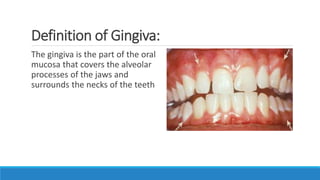
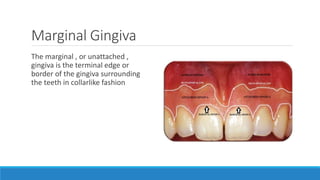
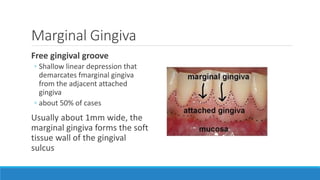
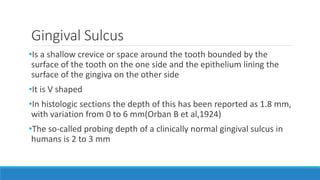
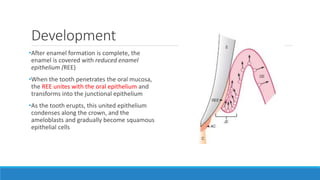
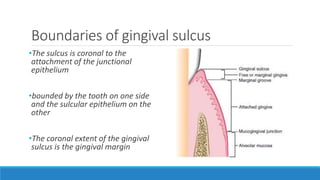
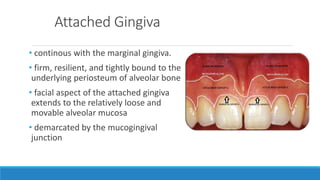
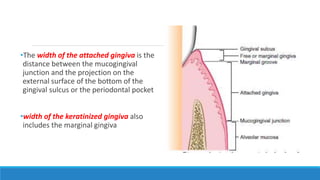
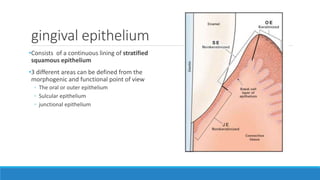
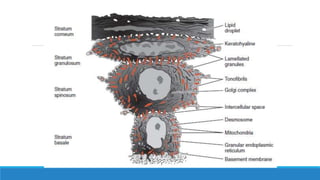
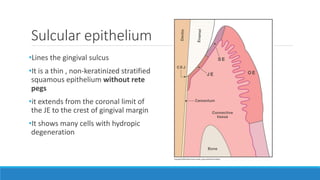
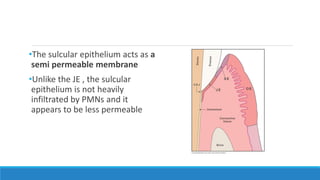
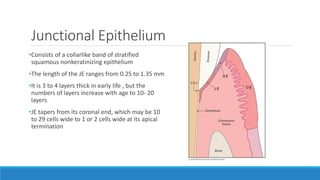
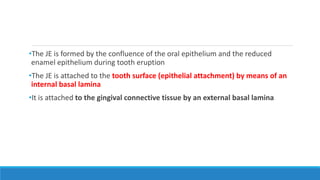
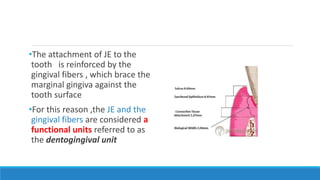
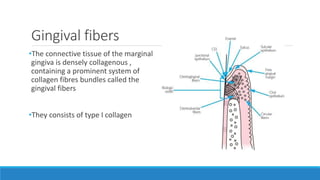
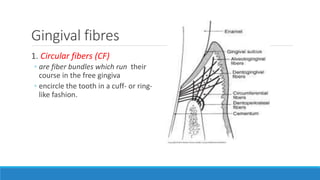
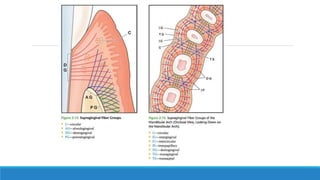
The gingiva is divided anatomically into the marginal, attached, and interdental gingiva. The marginal gingiva forms the soft tissue wall around the teeth. The attached gingiva is firmly bound to the underlying bone. The interdental gingiva occupies the spaces between teeth. Microscopically, the gingiva contains an epithelial layer and underlying connective tissue. The epithelial layer includes the sulcular, junctional, and oral epithelium. The connective tissue contains collagen, fibroblasts, and ground substance.