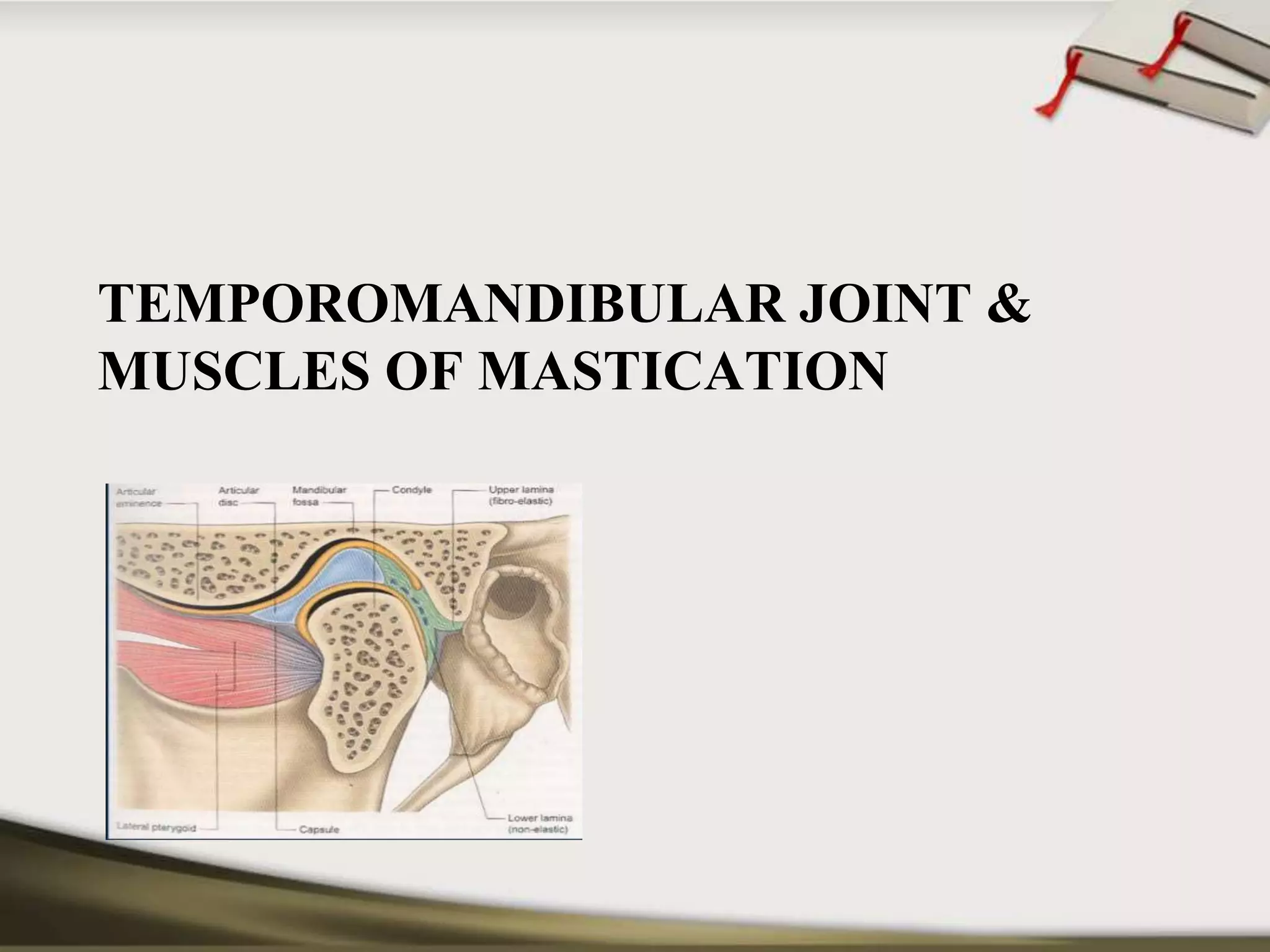
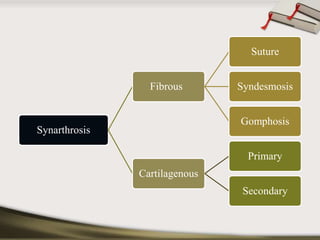
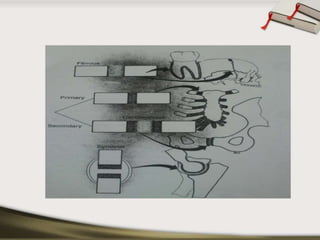
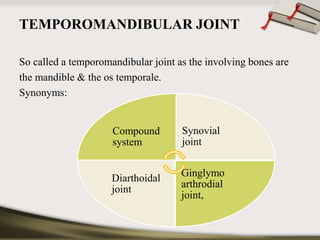
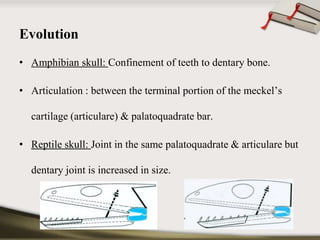
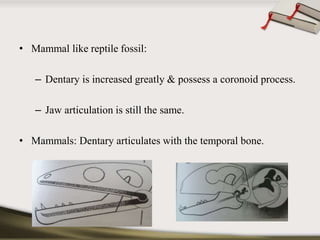
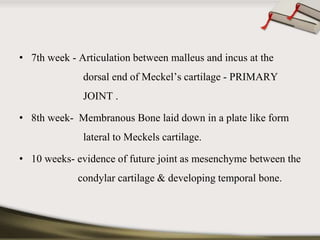
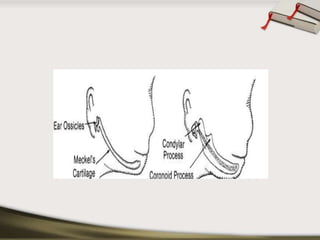
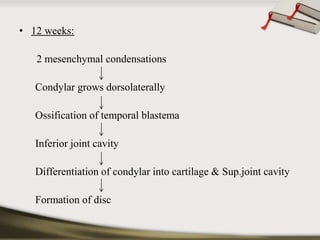
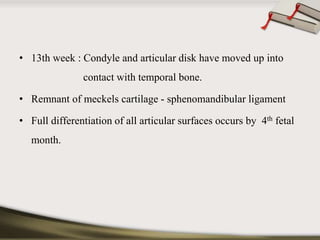
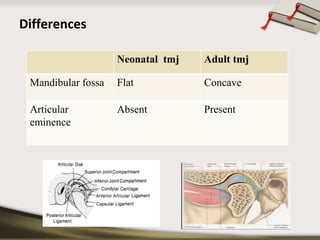
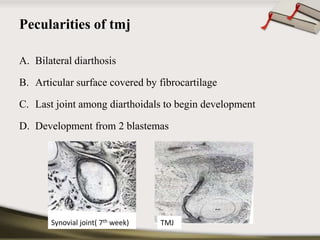
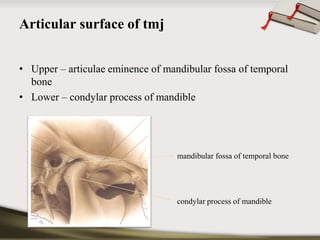
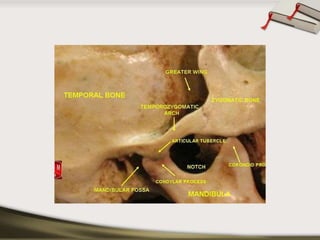
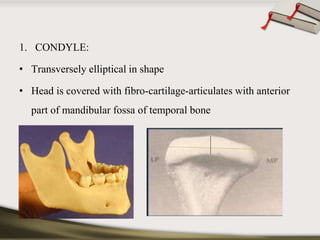
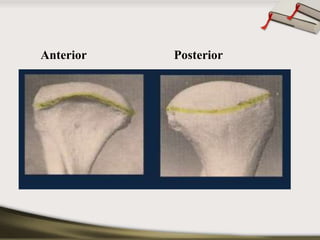
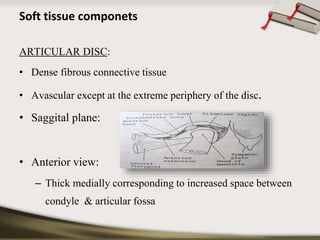
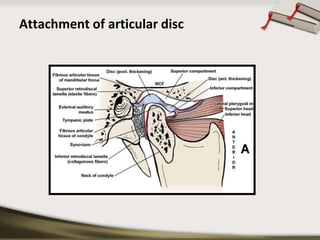
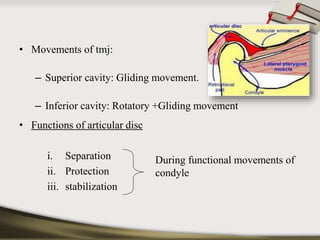
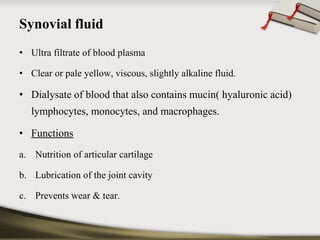
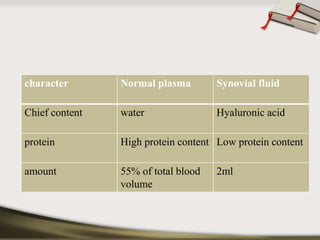
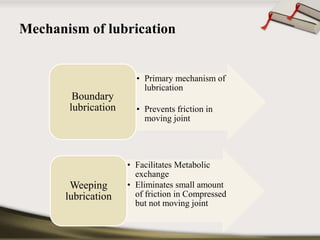
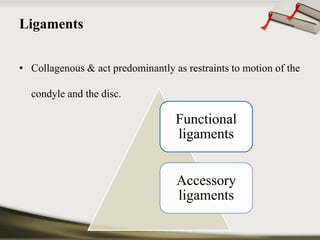
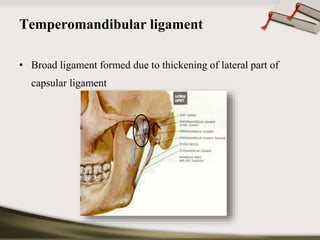
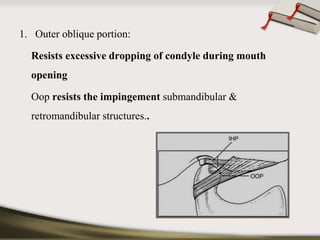
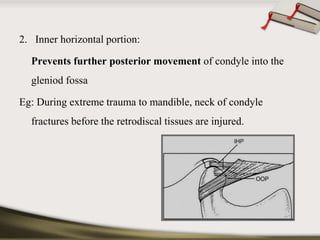
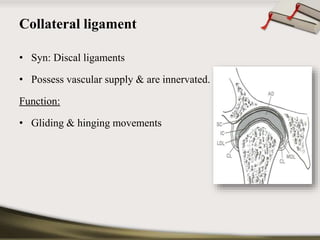
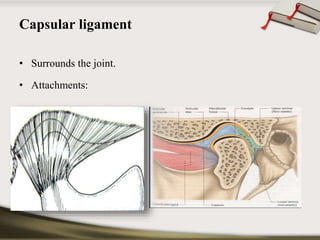
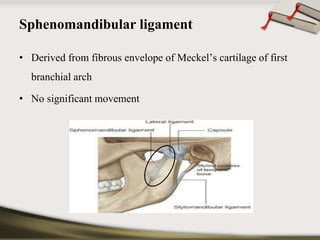
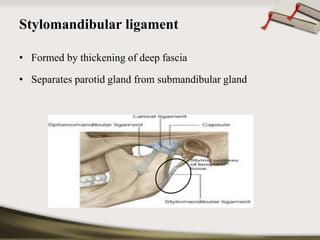
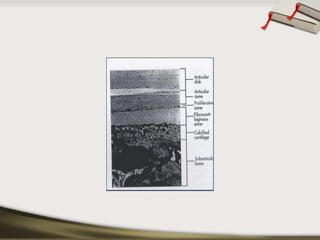
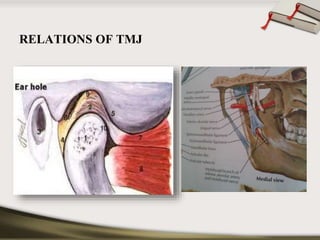
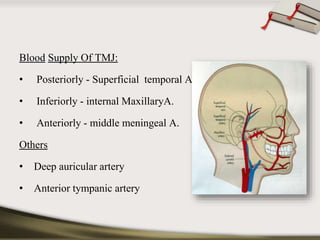
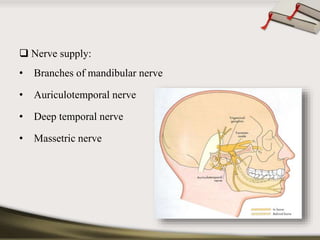
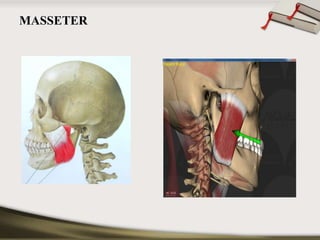
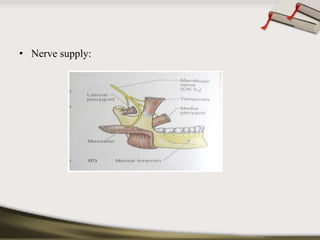
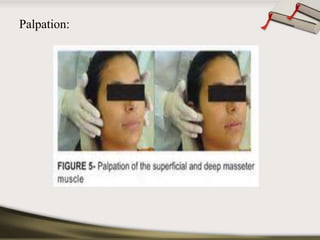
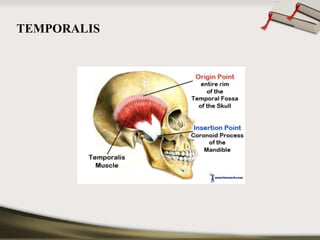
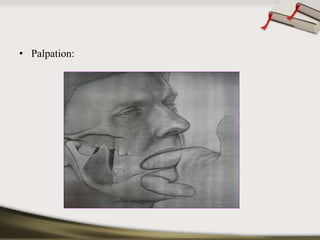
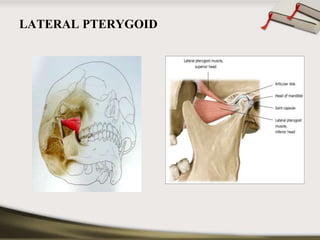
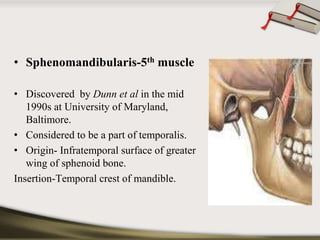
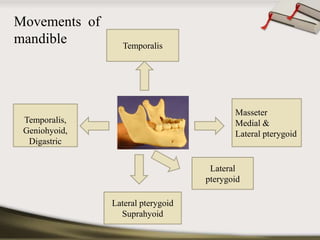
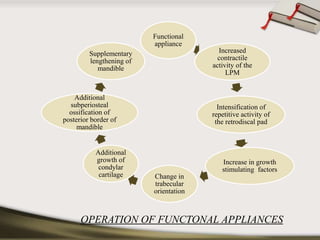
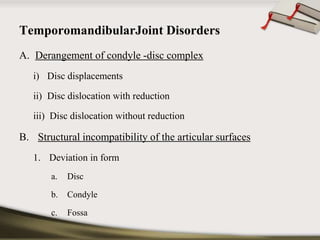
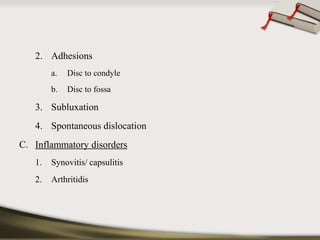
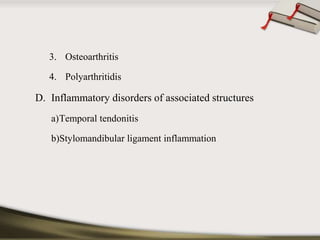
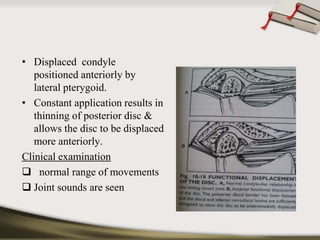
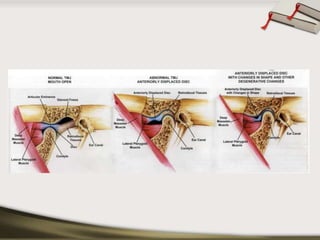
The document discusses the temporomandibular joint (TMJ) and muscles of mastication. It covers the evolution, embryology, anatomy, histology and biomechanics of the TMJ. The TMJ is a synovial diarthrodial joint that allows gliding and rotational movements. It involves the mandibular condyle articulating with the temporal bone. The muscles of mastication include the masseter, temporalis, medial pterygoid and lateral pterygoid muscles. Common TMJ disorders include disc displacements, derangements, and inflammatory conditions like synovitis, capsulitis and arthritis.