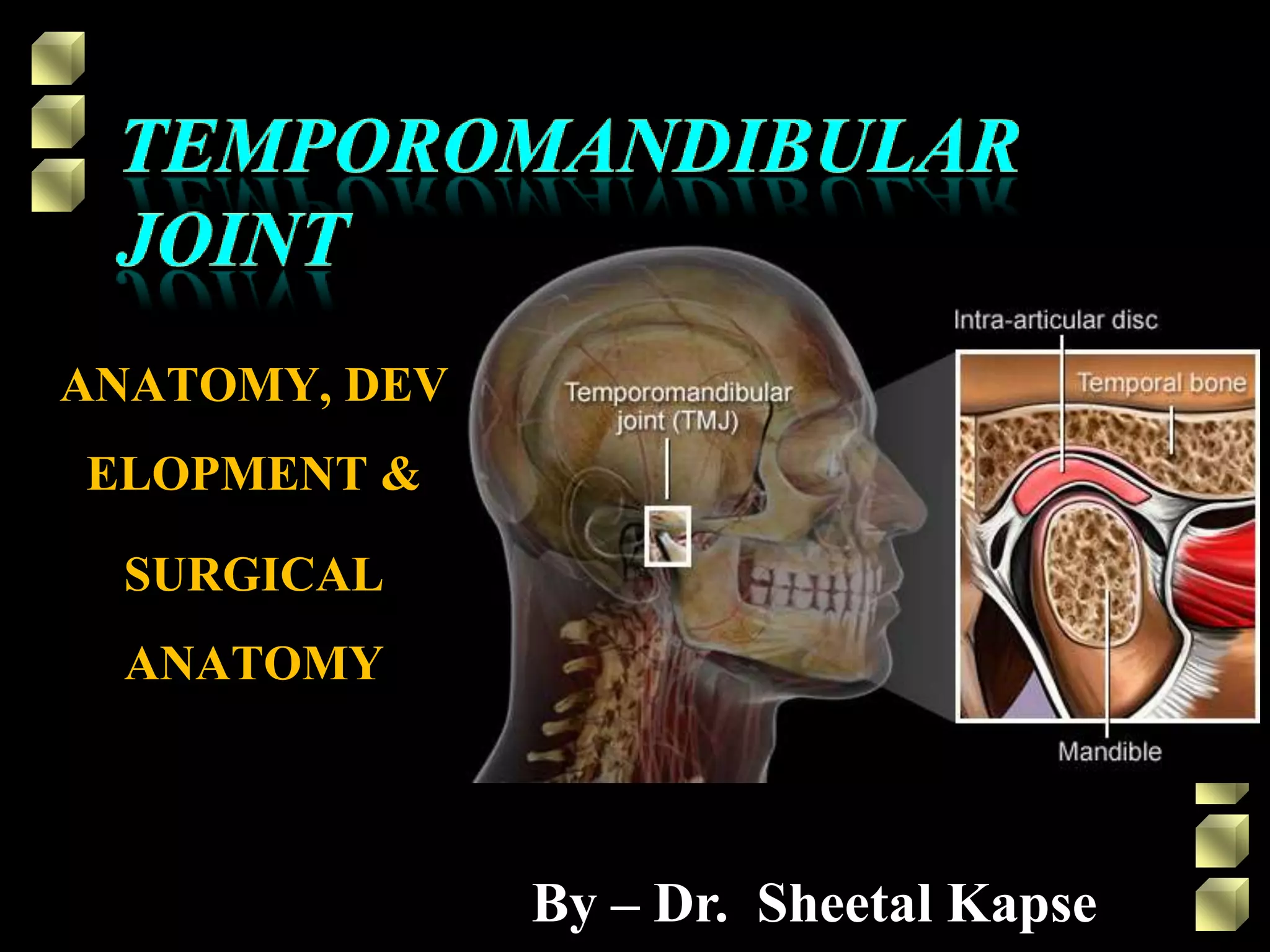
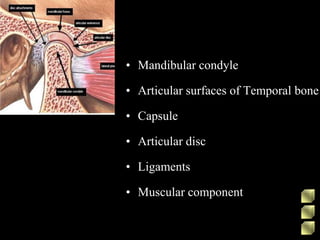
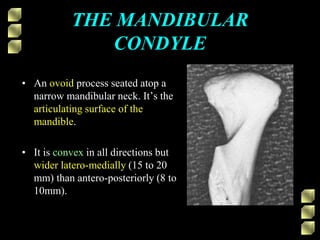
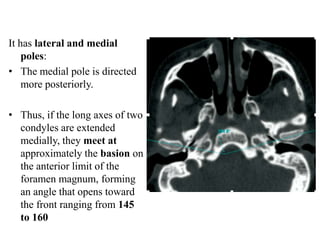
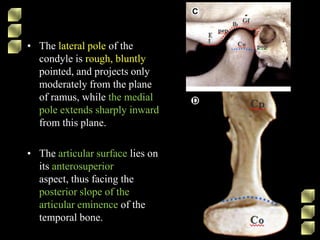
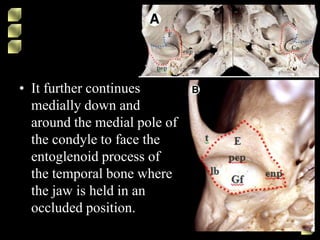
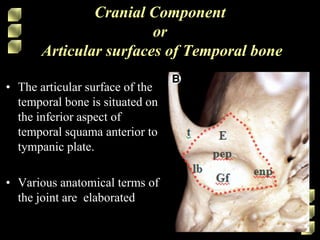
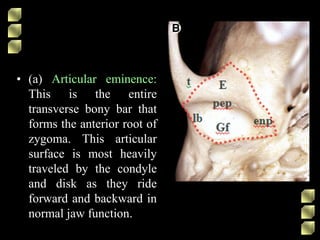
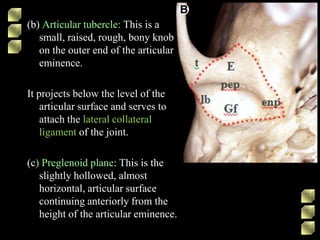
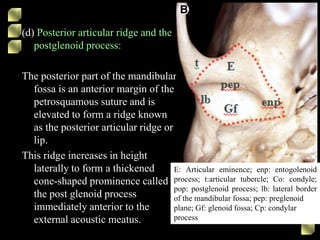
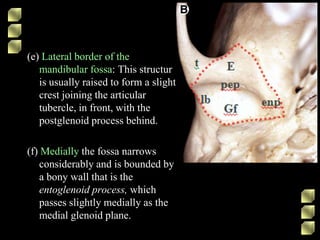
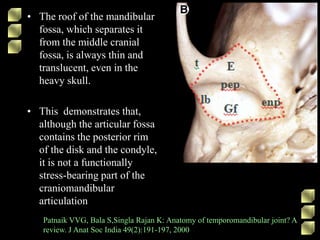
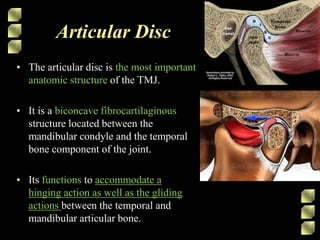
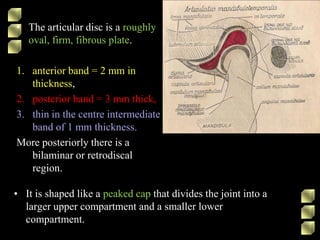
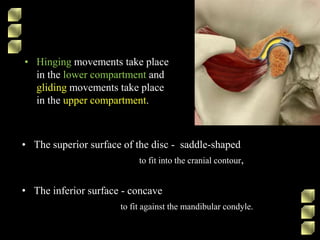
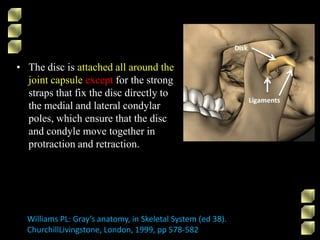
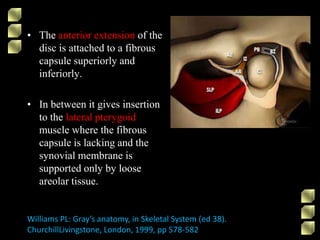
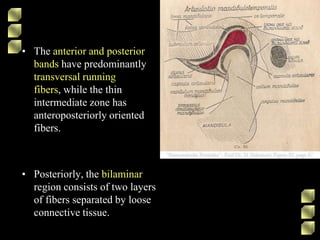
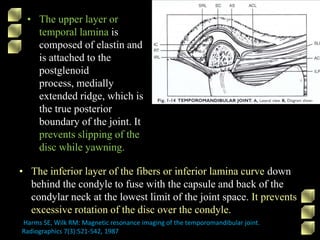
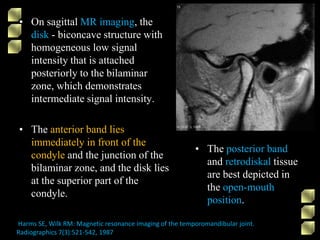
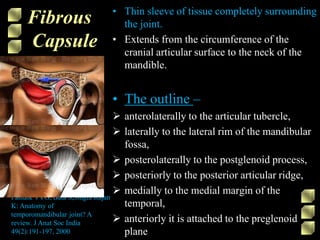
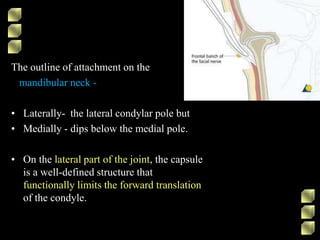
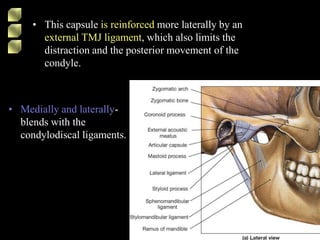
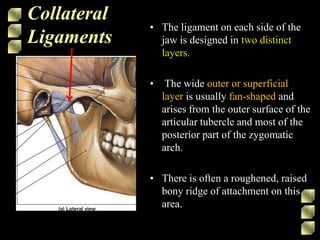
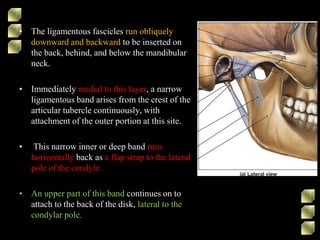
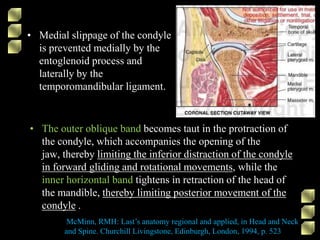
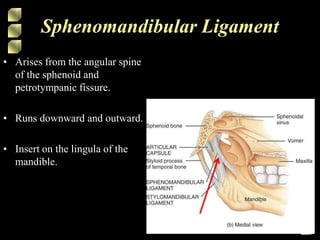
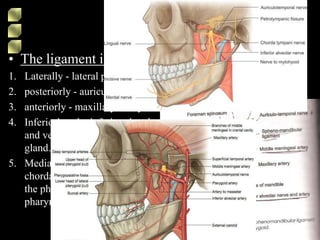
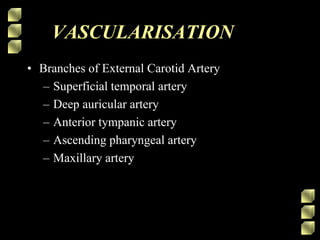
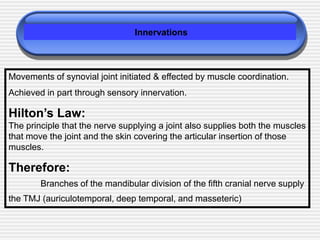
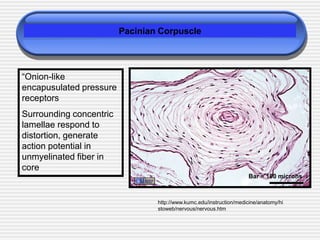
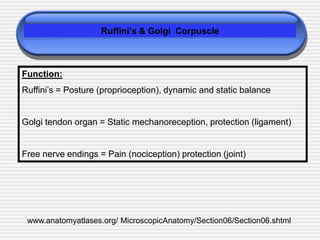
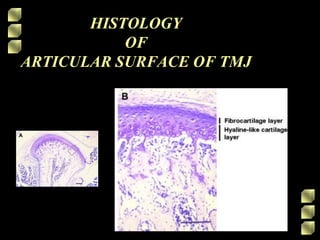
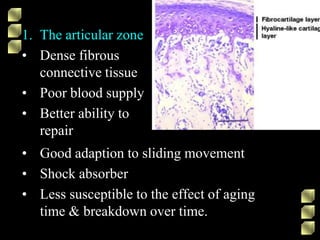
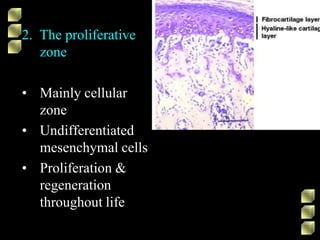
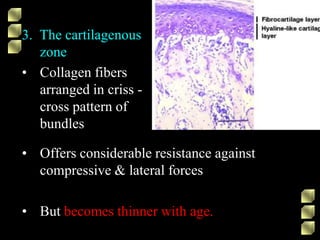
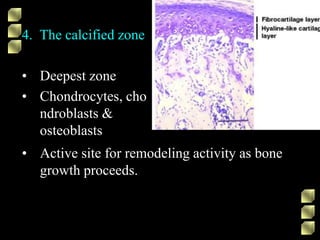
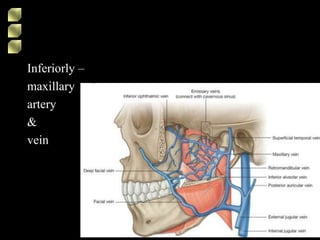
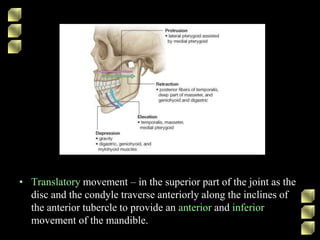
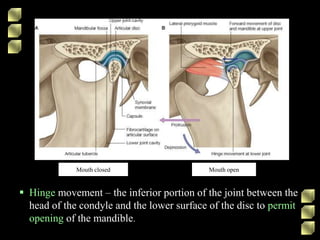
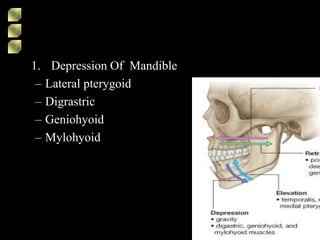
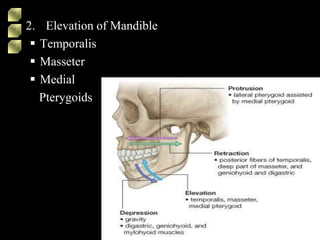
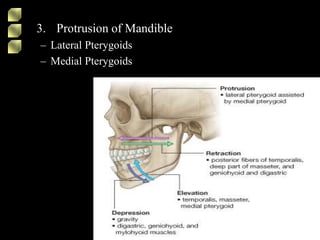
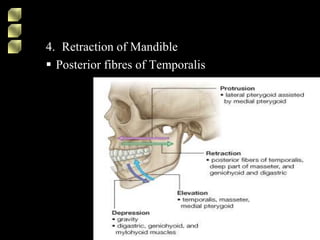
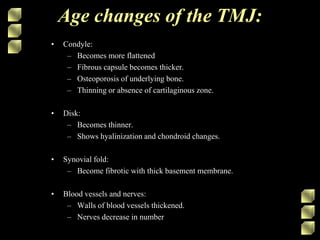
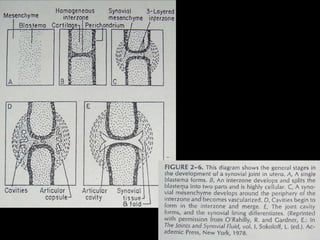
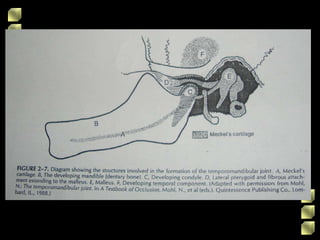
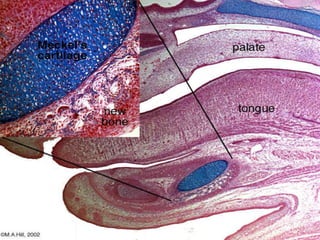
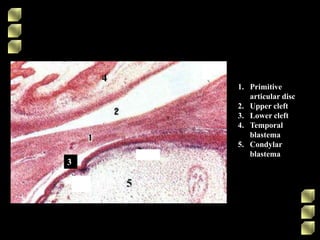
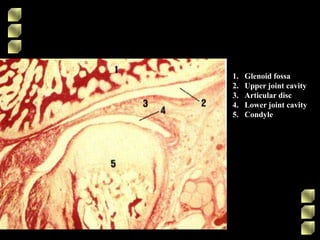
The document provides an overview of the anatomy, development, and surgical anatomy of the temporomandibular joint (TMJ). It discusses the key components of the TMJ, including the mandibular condyle, articular surfaces of the temporal bone, articular disc, fibrous capsule, and ligaments. It describes the development of the TMJ from two distinct blastemas beginning in the 7th week in utero. The document highlights several unique features of the TMJ, such as its articular surface being covered by fibrocartilage instead of hyaline cartilage. It also reviews the movements, vascular supply, innervation, and age-related changes of the TMJ.