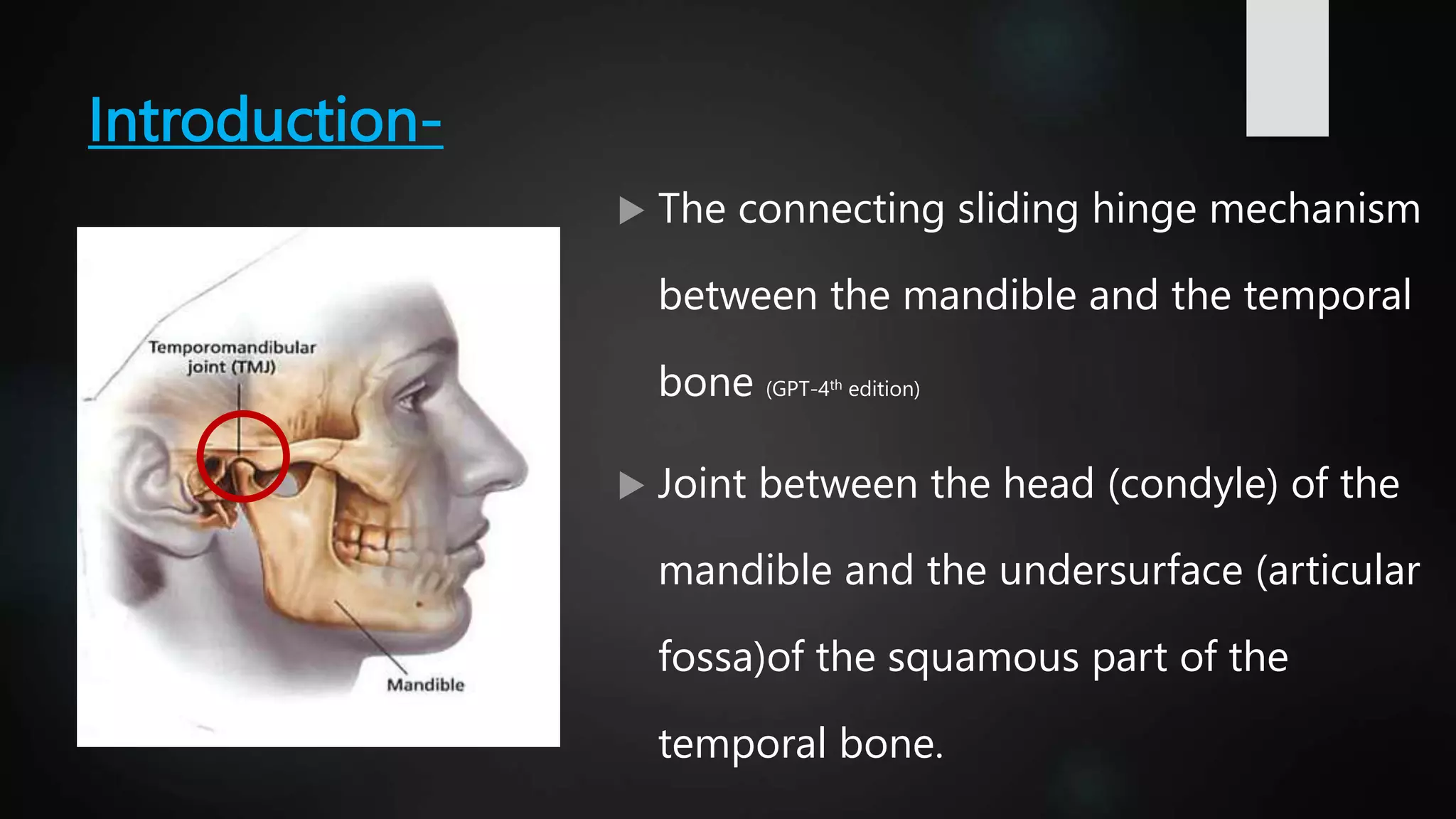
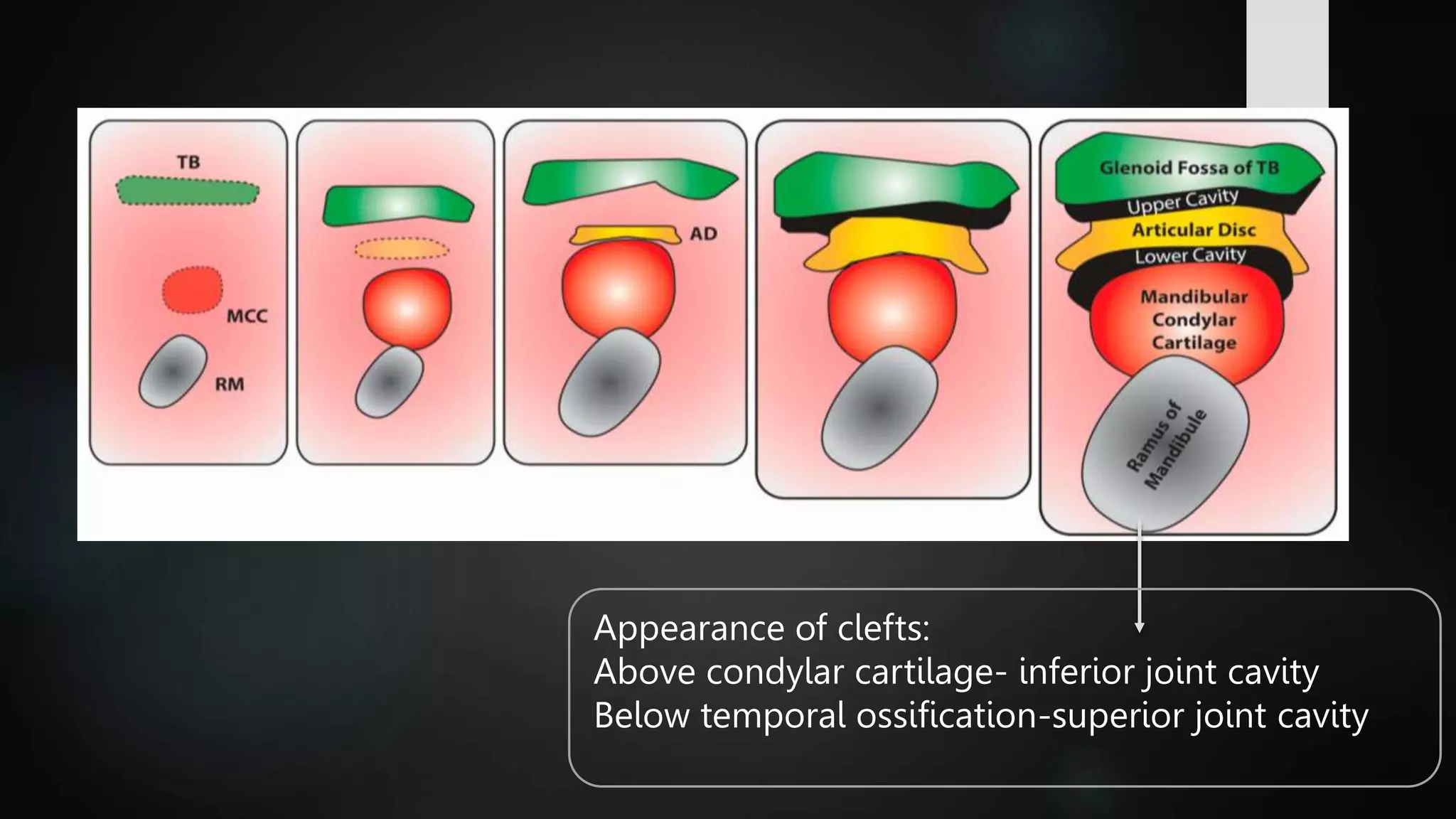
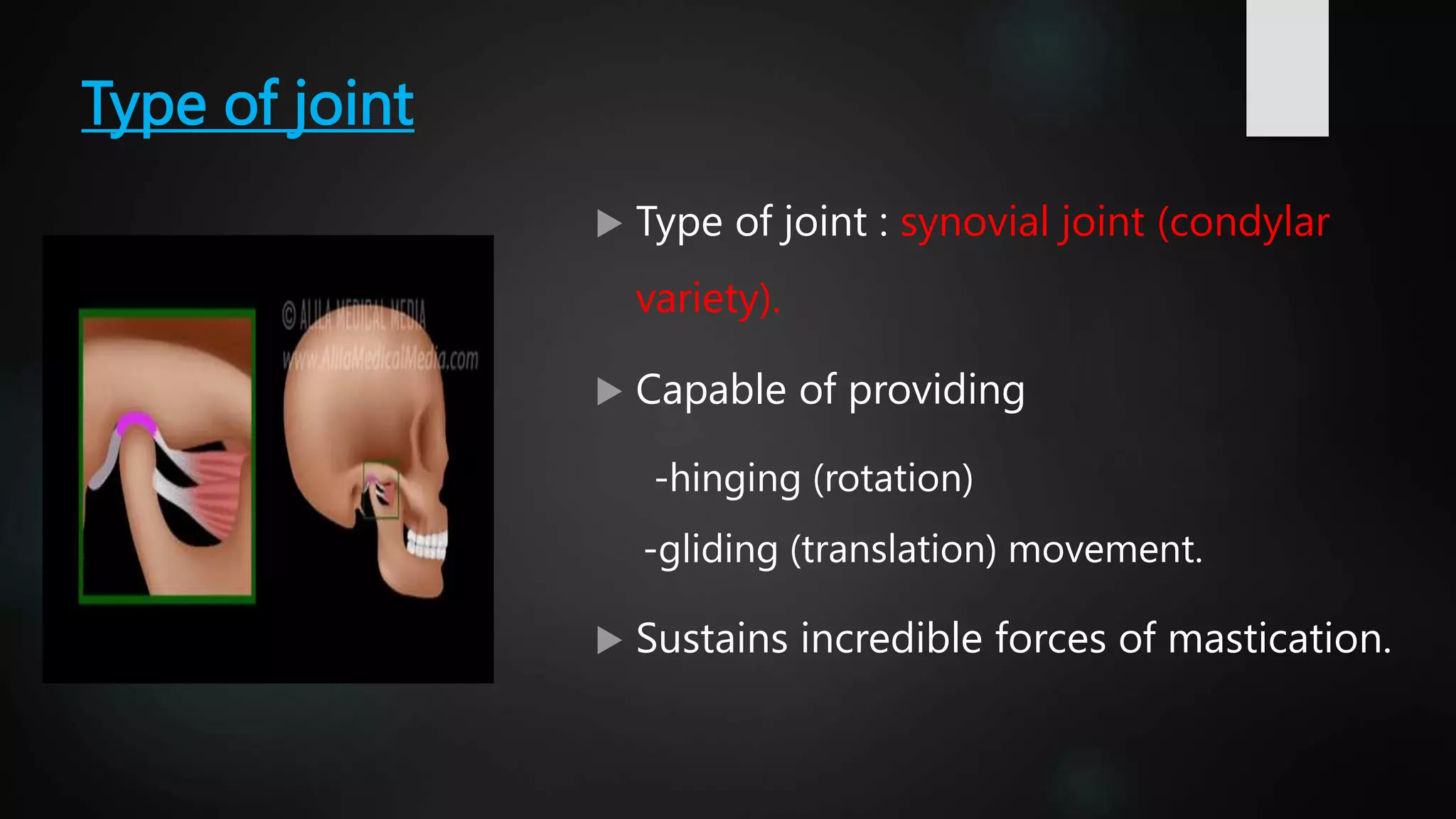
The document provides a detailed overview of the temporomandibular joint (TMJ), discussing its anatomical structure, development, types, functions, and clinical aspects. It covers aspects such as articular surfaces, ligaments, blood and nerve supply, various movements, and disorders associated with TMJ, including treatment approaches. Additionally, it addresses developmental anomalies and their implications for treatment.