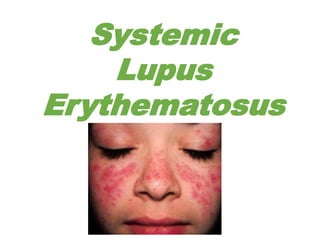
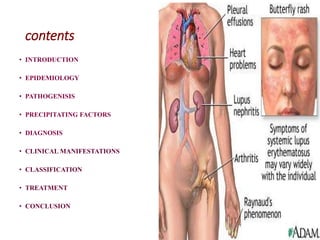
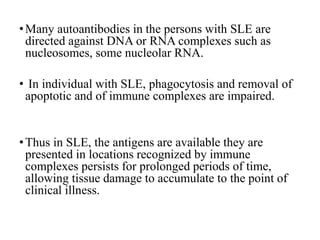
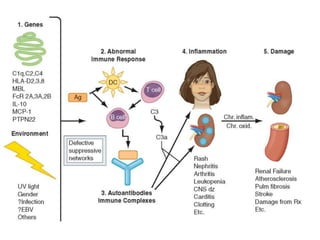
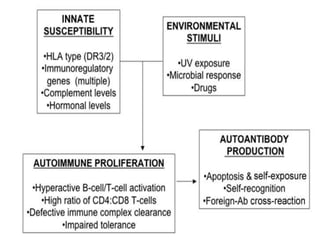
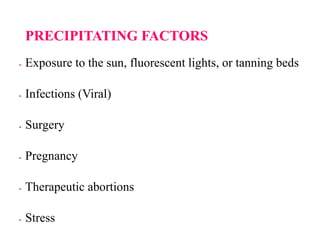
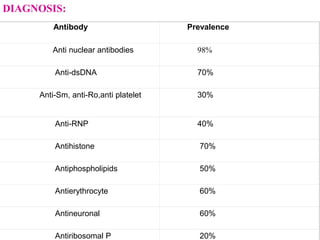
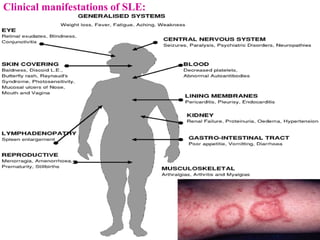
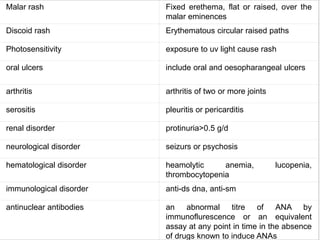
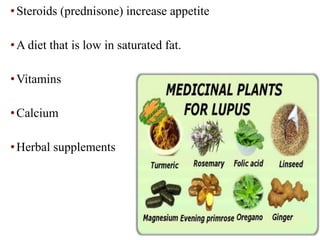
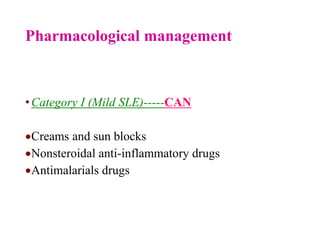
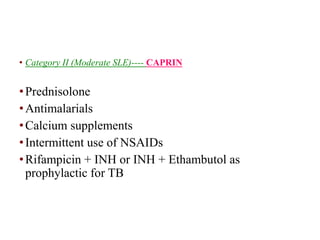
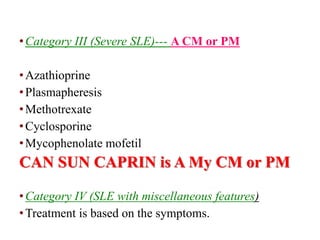
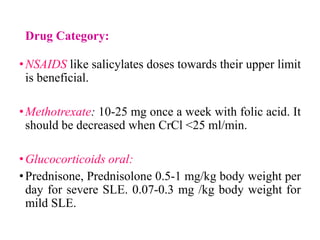
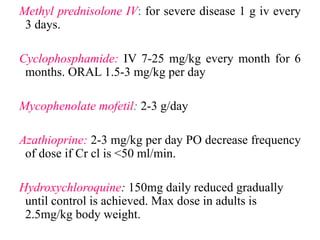
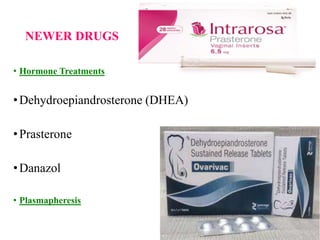
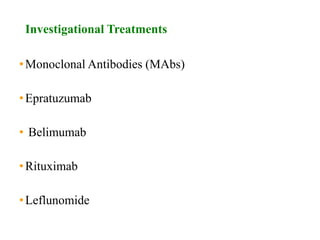
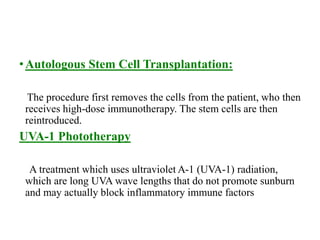
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease that can impact various body systems, with a higher prevalence in certain ethnic groups and females. The pathogenesis involves genetic and environmental factors leading to abnormal immune responses and tissue damage. Treatment focuses on managing symptoms and preventing flares, employing both pharmacological and non-pharmacological strategies, with ongoing research into new therapies.