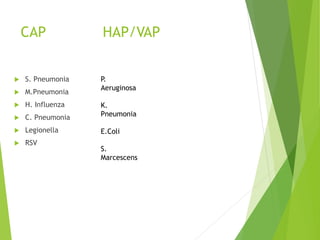
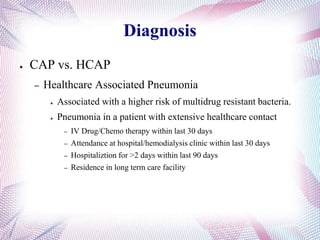
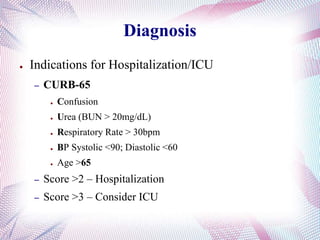
This document provides information about pneumonia, including epidemiology, common causes, diagnosis, treatment, and prevention. It notes that pneumonia affects over 3 million people annually in the US, with higher rates in winter and among males and those over 65. Diagnosis involves clinical assessment of symptoms and signs, with chest x-ray and testing to confirm. Treatment depends on location of acquisition and risk factors, starting with broad-spectrum antibiotics and later targeting likely pathogens. Prevention focuses on vaccination, especially for influenza and pneumococcus, and reducing risk factors like smoking.






















![CAP Treatment
● Empiric Outpatient
– Previously healthy patient
1.Macrolides (A.C.E) OR
2.Doxycycline
– Comorbidities, DM, Alcoholism, Immunosuppression,
Prior ABx use
1.Fluoroquinolones (-floxacins, [Levaquin]) OR
2.Beta-lactam(Amoxicillin/Ceftriaxone) AND Macrolides
● Consider Antipseudomonal for COPD](https://image.slidesharecdn.com/pneumonia-160322152143/85/Pneumonia-27-320.jpg)






