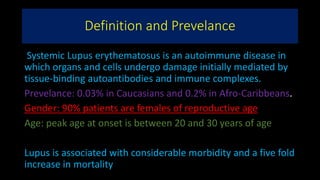
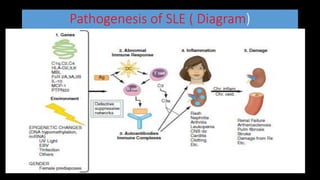
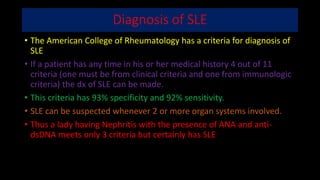
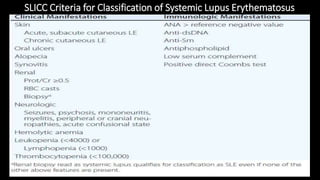
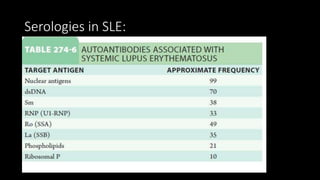
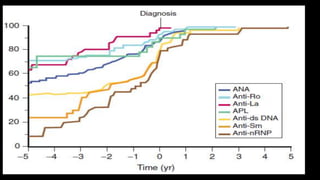
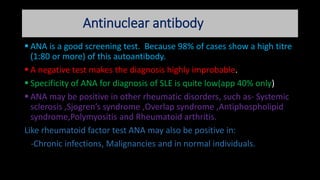
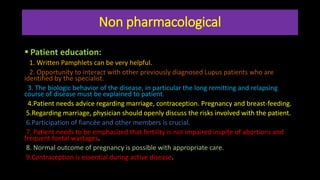
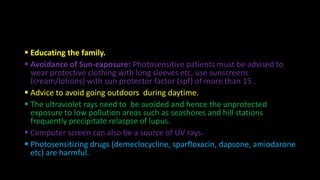
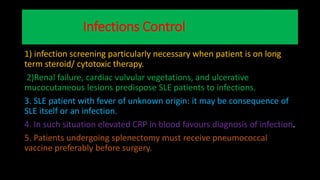
Systemic lupus erythematosus (SLE) is an autoimmune disease with a prevalence of 0.03% in Caucasians and 0.2% in Afro-Caribbeans, primarily affecting women of reproductive age. The disease is characterized by autoantibody production leading to various systemic symptoms and complications, including musculoskeletal, renal, and nervous system manifestations. Diagnosis is based on a combination of clinical criteria and serological tests, with management involving education, lifestyle modifications, and pharmacological treatments tailored to disease severity.