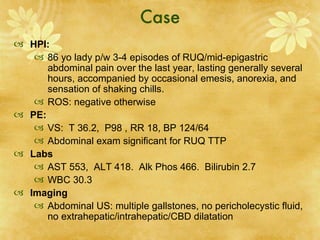
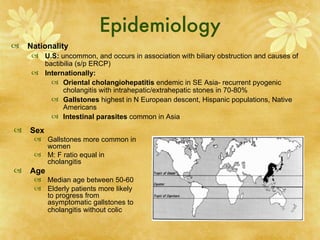
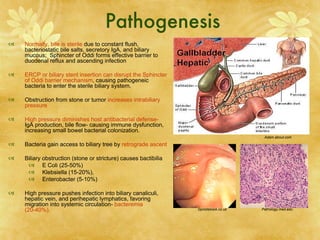
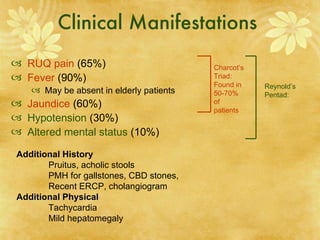
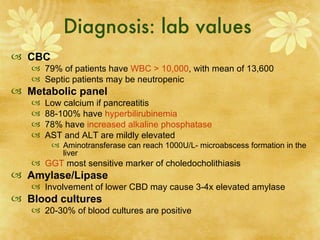
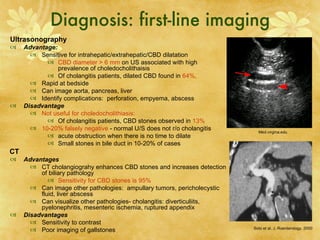
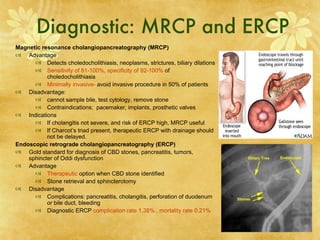
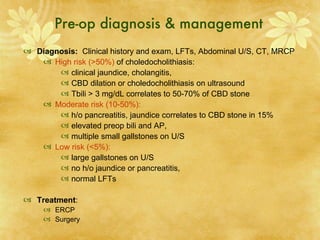
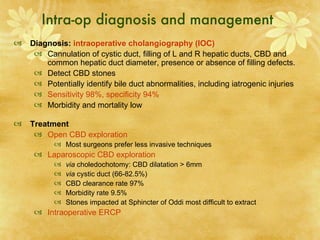
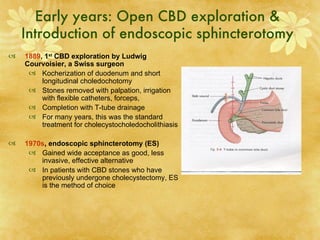
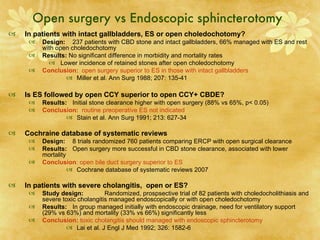
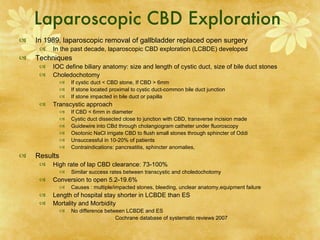
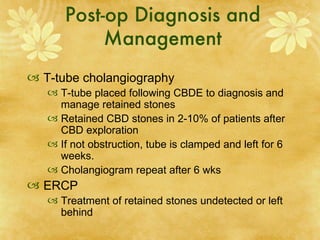
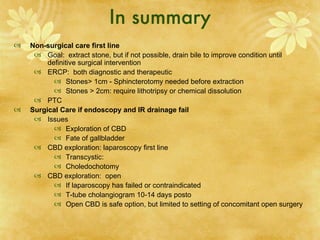
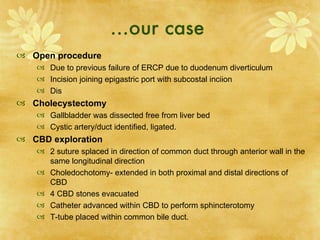
The document discusses cholangitis and choledocholithiasis, including their clinical manifestations, diagnosis, and various treatment approaches. It provides details on the pathogenesis, risk factors, diagnostic testing, and both medical and surgical management of these conditions, including endoscopic retrograde cholangiopancreatography (ERCP) and laparoscopic common bile duct exploration.