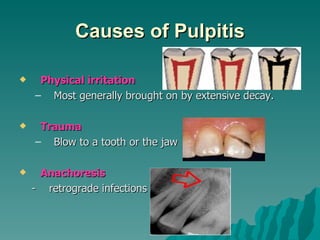
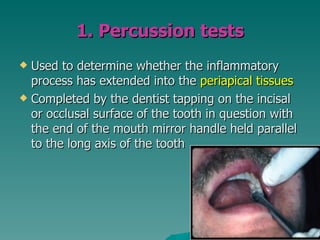
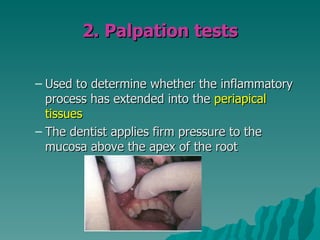
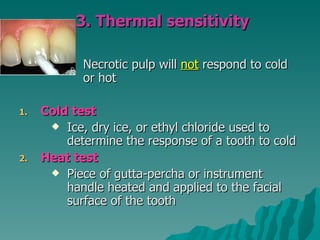
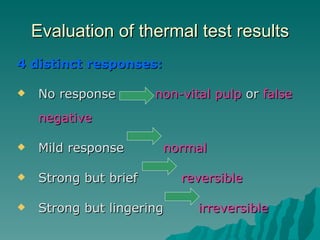
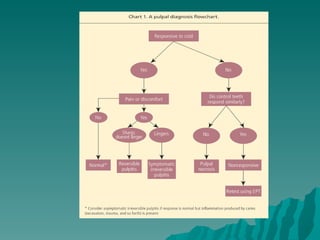
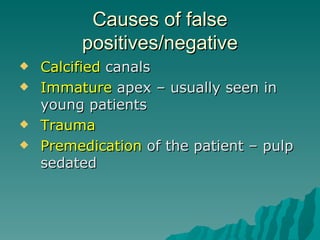
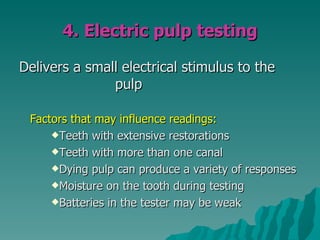
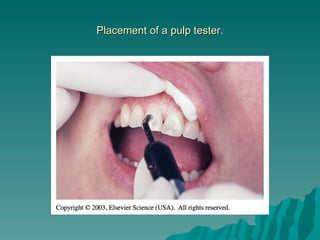
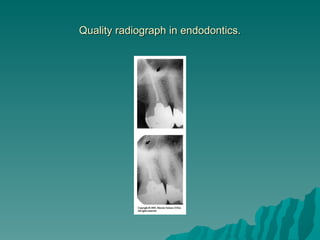
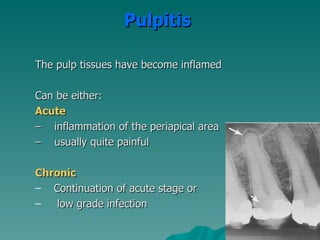
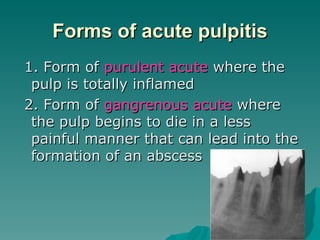
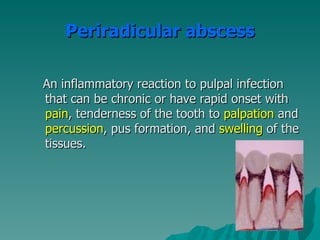
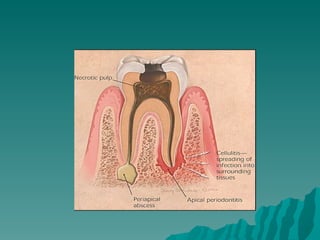
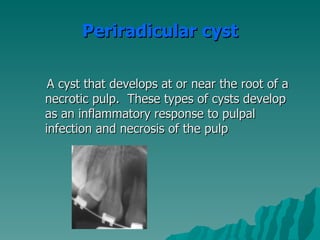
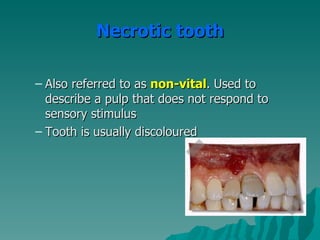
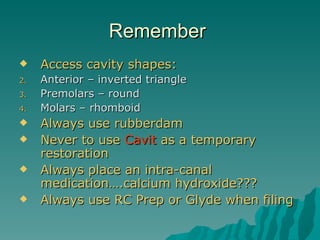
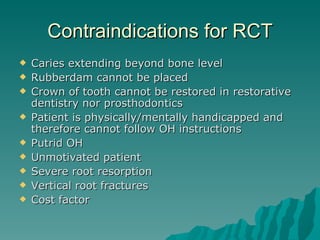
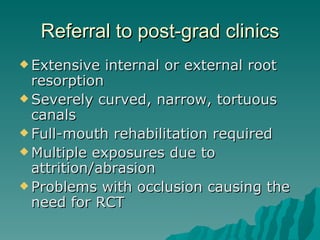
This document discusses endodontic diagnosis and treatment planning. It begins by introducing endodontics and describing common causes of pulpitis like decay, trauma, and infection. Signs and symptoms of pulpitis include tooth pain from hot/cold, pressure, and swelling. Diagnosis involves subjective questions to the patient and objective examination of the tooth. Diagnostic tests include percussion, palpation, thermal sensitivity testing, electric pulp testing, and radiographs. Based on the diagnostic findings, the dentist determines if the pulp is normal, inflamed with reversible or irreversible pulpitis, or non-vital. The treatment plan is tailored to the diagnosis but commonly involves accessing the root canal, cleaning and shaping it, and filling