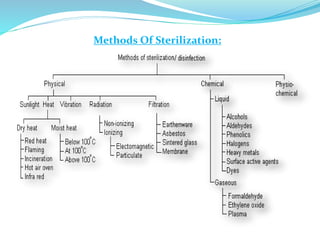
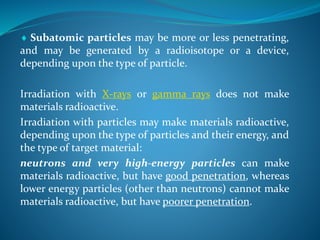
This document discusses various sterilization methods, including physical and chemical methods. Physical sterilization methods involve the use of heat, radiation, filtration, etc. to eliminate all life forms. Heat sterilization is one of the most common and reliable methods, and can be achieved through moist heat (e.g. autoclaving) or dry heat (e.g. hot air oven). Radiation sterilization uses ionizing radiation like gamma rays or X-rays to sterilize materials. The document provides details on the mechanisms, applications, and considerations of various physical sterilization techniques.

![HEAT:
Heat is considered to be most reliable method of sterilization
of articles that can withstand heat.
- acts by oxidative effects
Sunlight as the biggest source of heat is the oldest and
cheapest way of achieving partial sterilization of cloths.
- only bactericidal [kills only bacteria] in nature it is not
effective for a complete sterilization process.
- microbial activity of sunlight is due to the presence of UV
rays in it
- responsible for spontaneous sterilization by killing bacteria
suspended in water, provides natural method of disinfection of
water bodies such as tanks and lakes.](https://image.slidesharecdn.com/physicalsterlization-140426175249-phpapp02/85/Physical-sterlization-6-320.jpg)

![Hot Air Oven:
•This method was introduced by Louis Pasture.
•Articles to be sterilized are exposed to high temperature
[160°c] for duration of 1-2 hour in an electrically heated oven.
•Since air is poor conductor of heat, even distribution of heat
throughout the chamber is achieved by a fan.
•The heat is transferred to the article by radiation,
conduction and convection.](https://image.slidesharecdn.com/physicalsterlization-140426175249-phpapp02/85/Physical-sterlization-22-320.jpg)
![• Consist of three walls and a door made of gun metal that
insulate and keep the heat in and conserves energy, the inner
layer being a poor conductor and outer layer being metallic.
-air filled space in between to aid insulation.
• An air circulating fan helps in uniform distribution of the heat.
• These are fitted with the adjustable wire mesh plated trays or
aluminum trays and may have an on/off rocker switch, as well as
indicators [thermostat] and controls for temperature and
holding time](https://image.slidesharecdn.com/physicalsterlization-140426175249-phpapp02/85/Physical-sterlization-23-320.jpg)

![Sterilization Control:
• Three methods exist to check the efficacy of sterilization
process, namely physical chemical and biological.
Physical – Temperature chart recorder and thermocouple.
Chemical – Browne’s tube No.3 [green spot, color changes
from red to green]
Biological – 10^6 spores of Bacillus subtilis or Clostridium
tetani on paper strips are placed inside the hot air oven.
After sterilization cycle, the strips are inoculated into
thioglycollate broth or cooked meat medium and incubated at
37°c for 3-5 days.
Proper sterilization NO GROWTH](https://image.slidesharecdn.com/physicalsterlization-140426175249-phpapp02/85/Physical-sterlization-27-320.jpg)
![At temperature below 100°c:
Pasteurization:
•This process was originally employed by Louis Pasteur.
•Currently this procedure is employed in food and dairy
industry.
• There are two methods of pasteurization,
holder method [heated at 63°c for 30 minutes]
flash method [heated at 72°c for 15sec.] followed by quickly
cooling to 13°c.](https://image.slidesharecdn.com/physicalsterlization-140426175249-phpapp02/85/Physical-sterlization-30-320.jpg)
![• Other pasteurization method include Ultra-High
temperature [UHT], 140°c for 15sec and 149°c for .5sec.
•This method is suitable to destroy most milk borne
pathogens like Salmonella, Mycobacteria, and
Streptococoi.
Efficacy is tested by phosphatase test and methylene
blue test.](https://image.slidesharecdn.com/physicalsterlization-140426175249-phpapp02/85/Physical-sterlization-31-320.jpg)
![Advantage of Steam:
• more penetrative power than dry air
• moistens the spores [moister is essential for
coagulation of proteins],](https://image.slidesharecdn.com/physicalsterlization-140426175249-phpapp02/85/Physical-sterlization-35-320.jpg)
![• Energy transmitted through space in a variety of forms is generally
called Radiation.
•Electromagnetic radiation can interact with matter in one of 2
general ways:
IONIZING RADIATIONS [X-ray and Y-rays]
NON-IONIZING RADIATION [UV light]](https://image.slidesharecdn.com/physicalsterlization-140426175249-phpapp02/85/Physical-sterlization-46-320.jpg)

![When ingredients of a culture medium are thermolabile. i.e.,
destroyed by heat, the use of heat sterilization is not
practicable.
In such cases, however, the process of filtration is used.
[biological fluids such as solutions of antibiotics, vitamins,
tissue extracts, animal serum, etc.]](https://image.slidesharecdn.com/physicalsterlization-140426175249-phpapp02/85/Physical-sterlization-54-320.jpg)

![HEPA Filter:
High- Efficiency Particulate Air [HEPA]
Filter has made it possible to deliver clean air
to an enclosure such as a cubicle or a room.
This type of air filtration together with a
system of Laminar Airflow is now extensively
used to produce dust and bacteria free air](https://image.slidesharecdn.com/physicalsterlization-140426175249-phpapp02/85/Physical-sterlization-61-320.jpg)

![Temperature below the optimum for growth depresses the rate
of metabolism, and if the temperature is sufficiently low, growth
and metabolism ceases.
Low temperature is useful for preservation of cultures, since
microorganism have a unique capacity for surviving extreme
cold. [-20 -70°c]
Liquid Nitrogen at a temperature of -196°c is used for
preserving cultures
In all these procedures, the initial freezing kills a fraction of
population, but the survivors may remain viable for long
periods.](https://image.slidesharecdn.com/physicalsterlization-140426175249-phpapp02/85/Physical-sterlization-63-320.jpg)