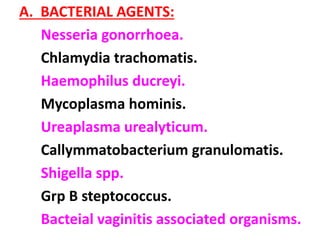
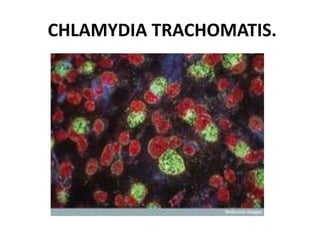
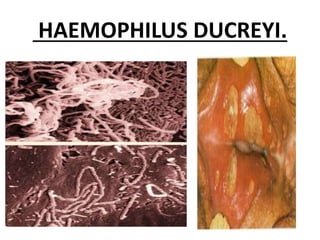
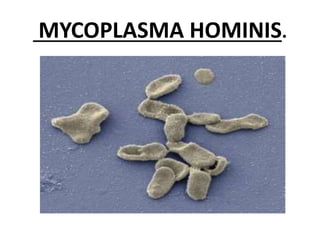
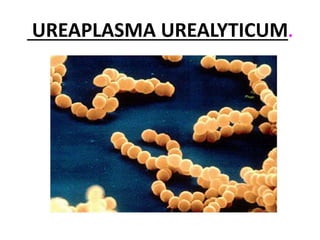
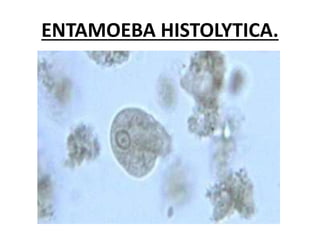
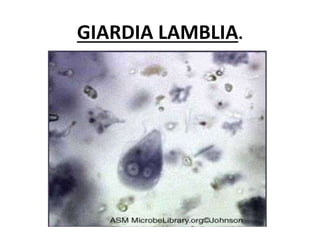
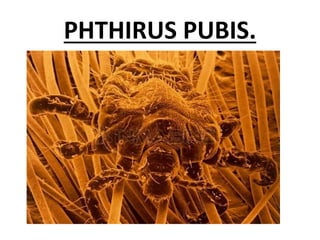
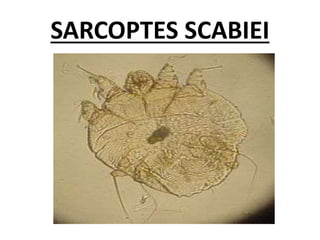
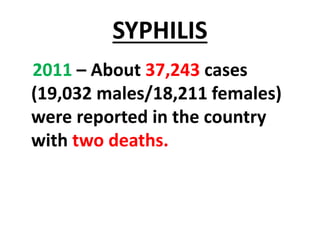
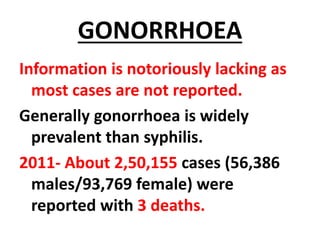
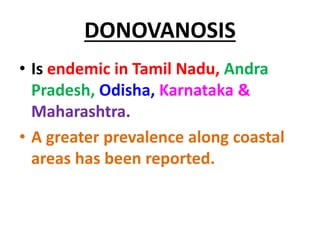
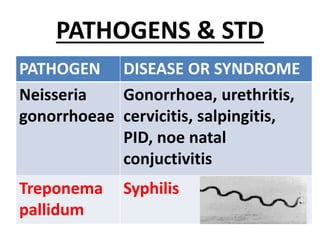
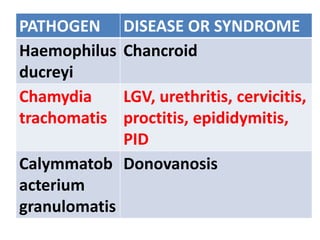
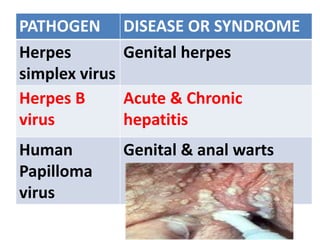
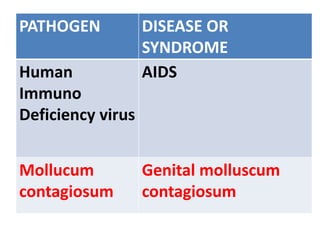
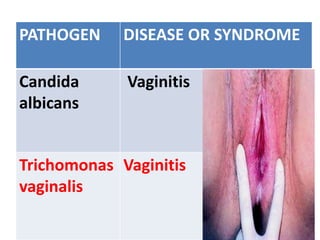
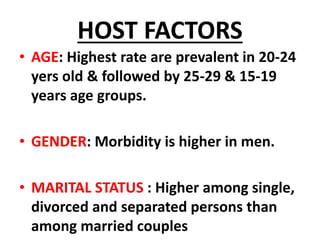
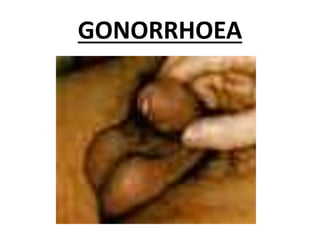
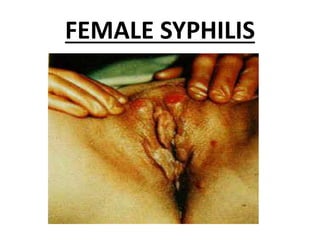
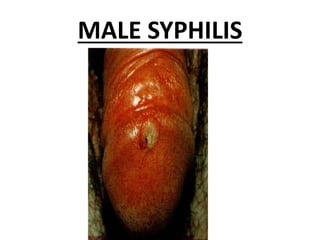
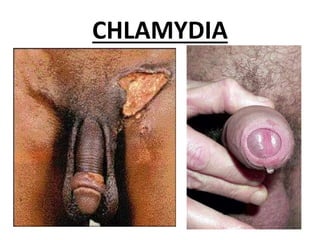
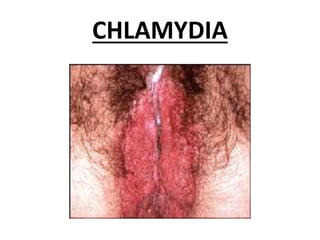
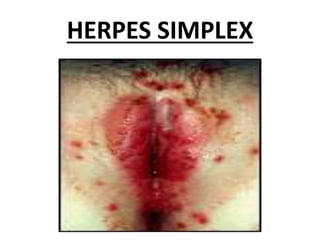
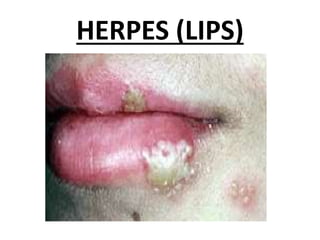
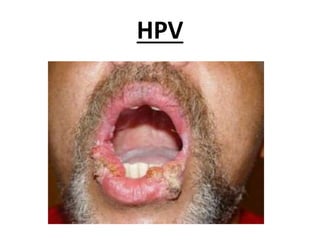
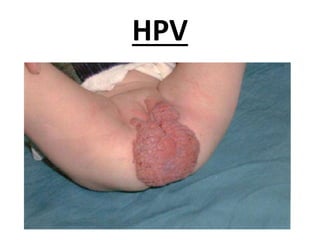
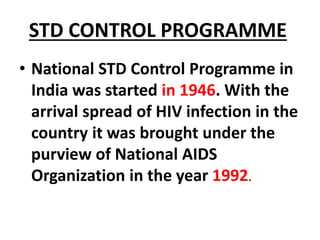
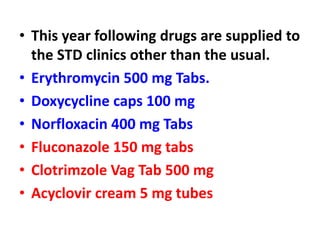
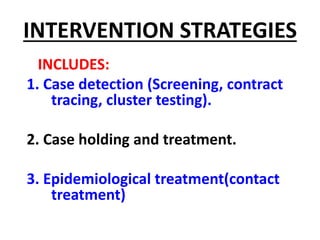
This document discusses sexually transmitted diseases (STDs) including their causes, symptoms, and treatment. It notes that STDs are predominantly spread through sexual contact and can be caused by bacteria, viruses, parasites or fungi. Common STDs mentioned include gonorrhea, chlamydia, syphilis, herpes, HIV/AIDS, and human papillomavirus. The document also addresses classification of STD agents, prevalence of STDs globally and in India, risk factors, control programs, and treatment options.