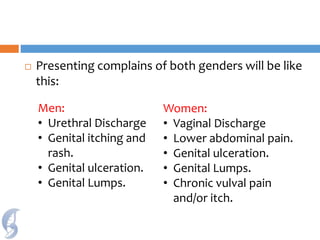
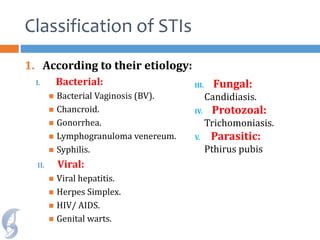
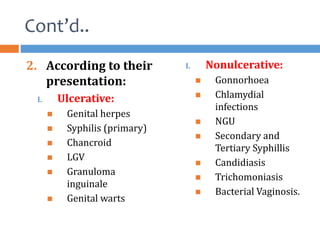
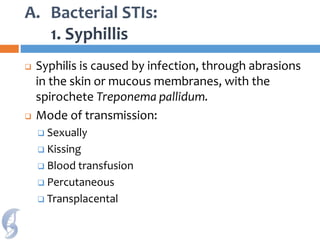
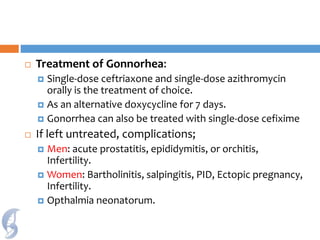
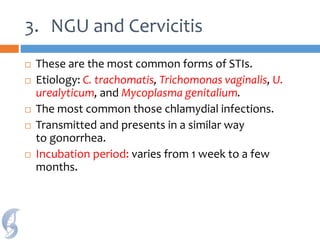
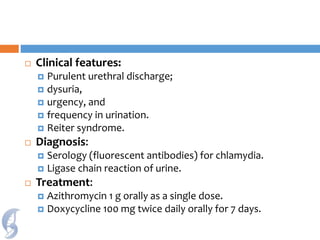
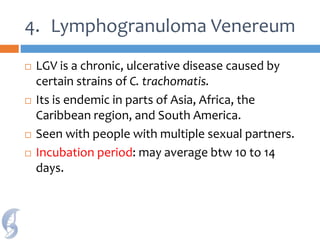
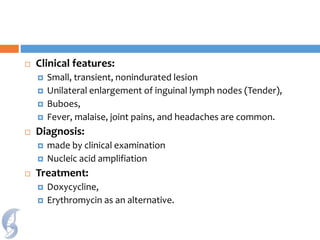
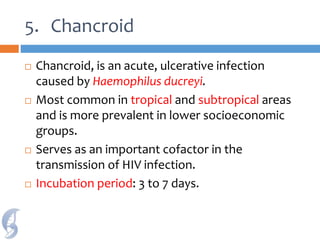
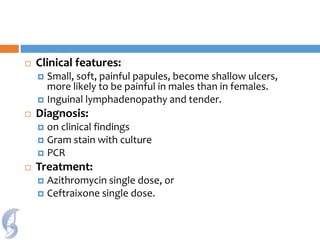
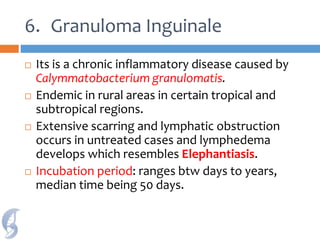
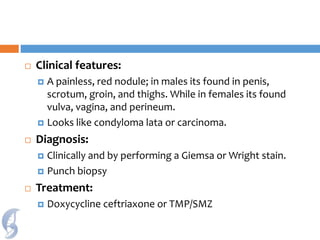
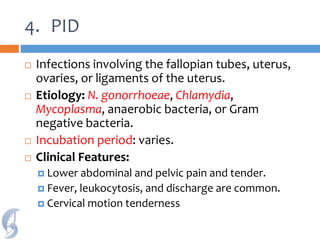
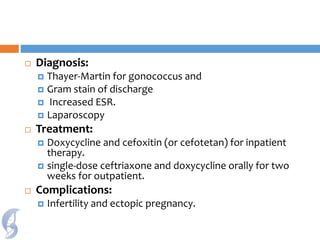
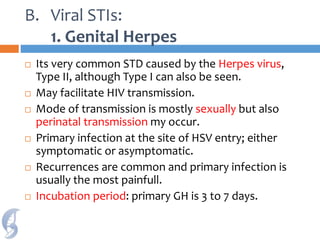
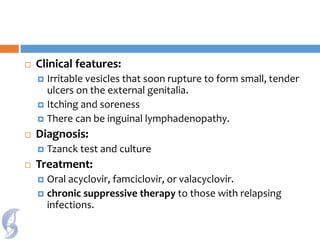
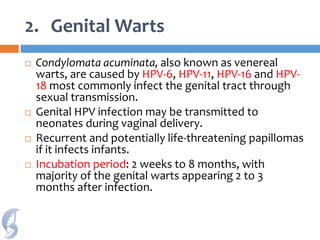
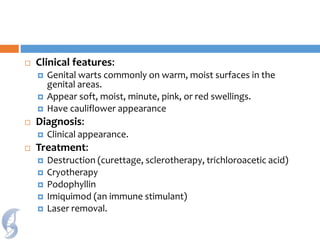
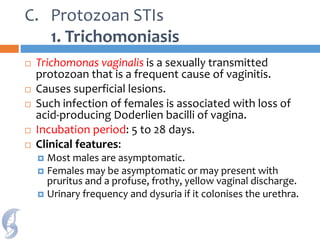
This document discusses sexually transmitted infections (STIs). It provides an overview of common STIs including bacterial STIs like syphilis, gonorrhea, chlamydia, and viral STIs like genital herpes and genital warts. It describes the causative agents, modes of transmission, symptoms, diagnoses and treatments for each STI. The document also discusses protozoan STIs like trichomoniasis. Overall, the document serves as an informative reference on the principal sexually transmitted infections, their characteristics, and clinical management.