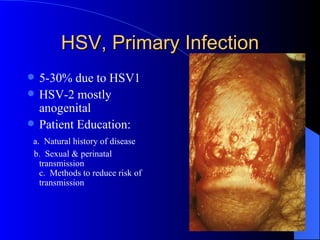
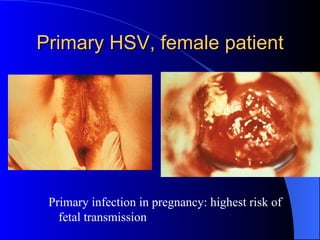
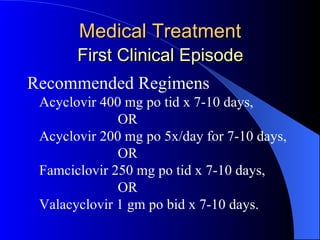
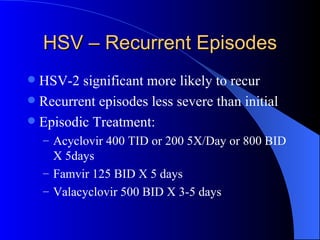
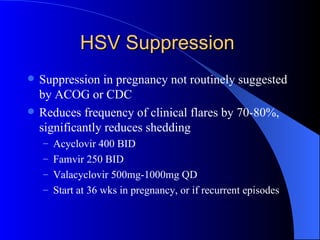
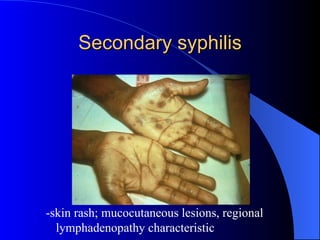
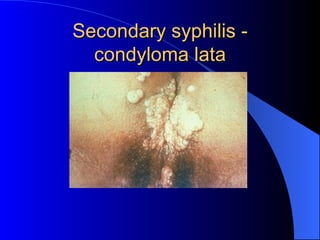
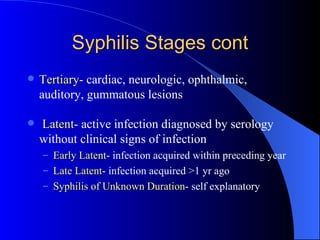
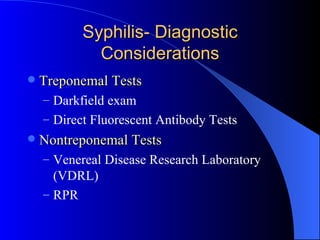
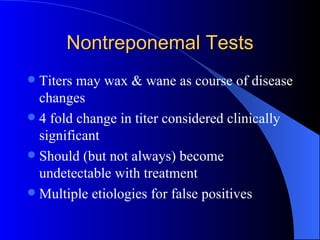
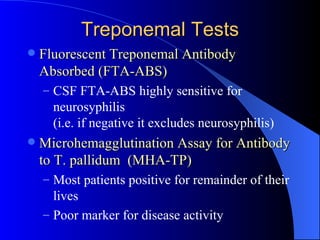
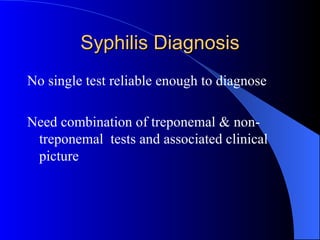
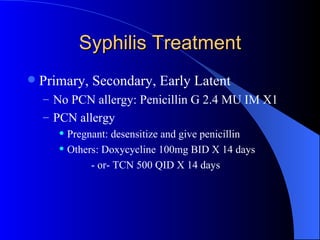
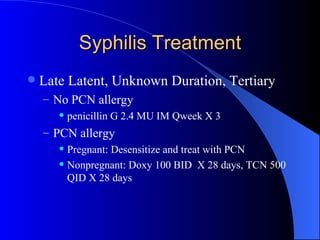
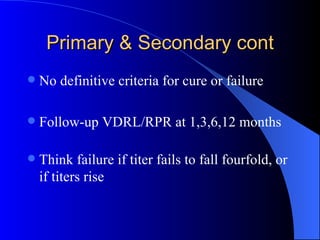
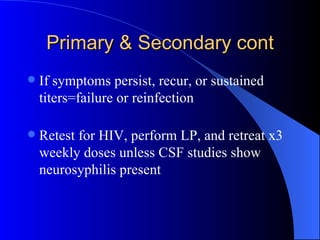
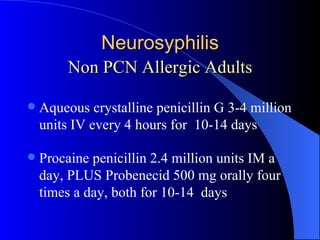
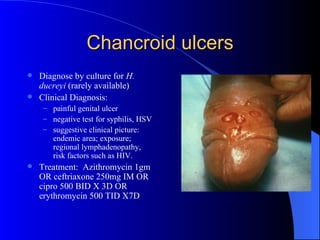
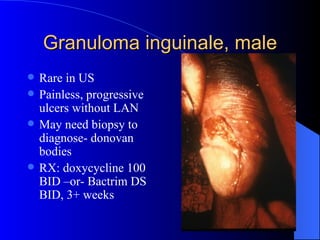
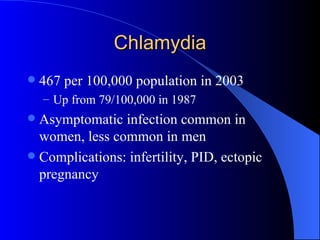
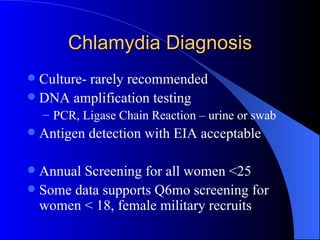
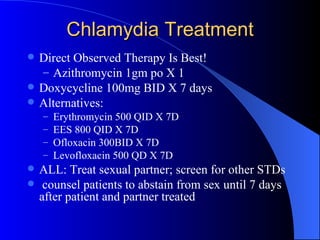
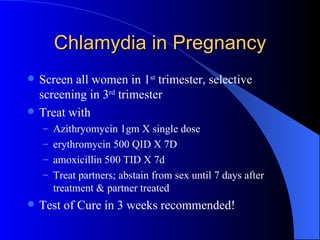
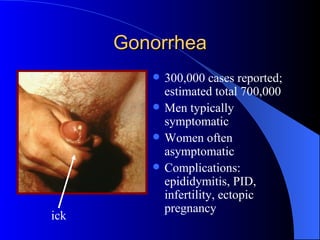
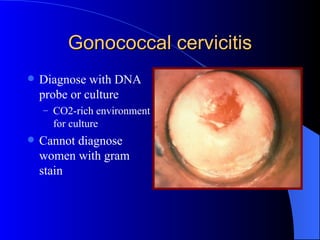
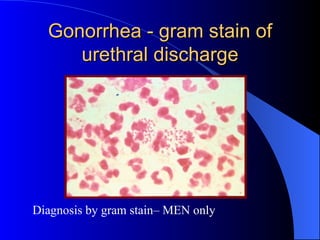
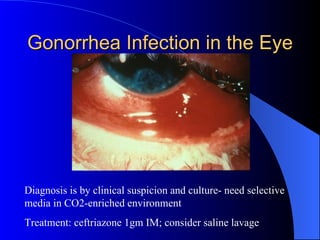
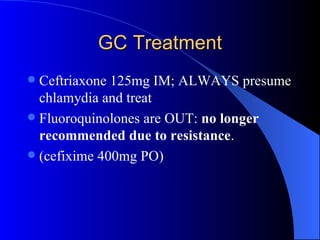
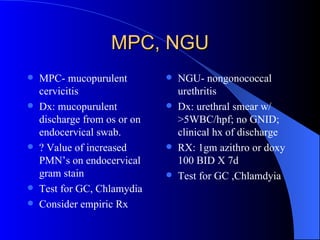
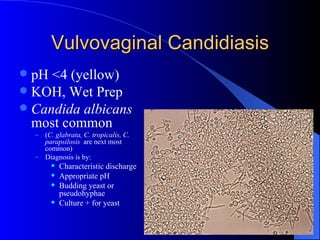
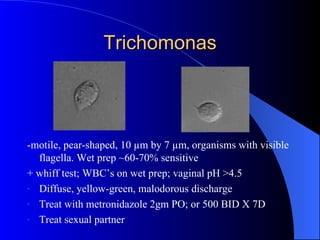
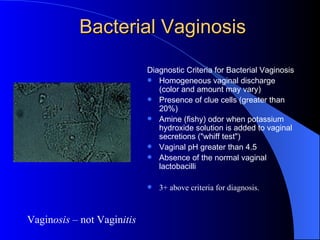
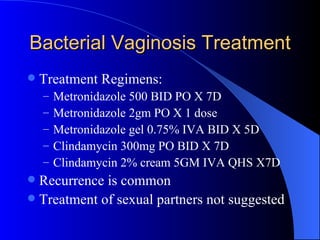
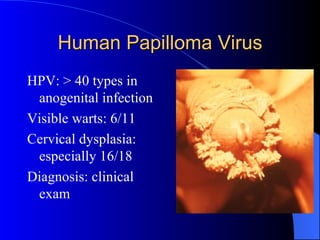
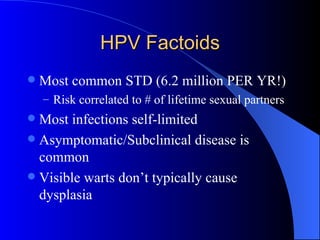
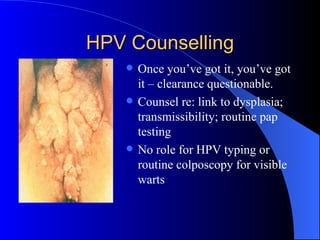
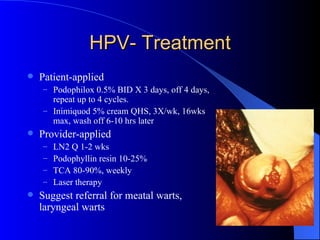
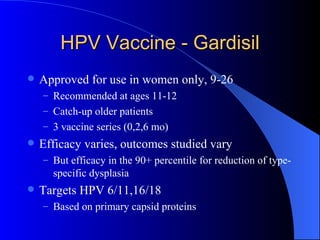
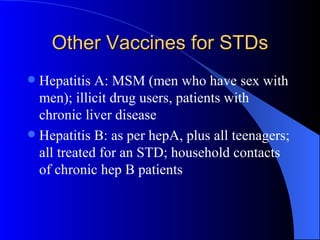
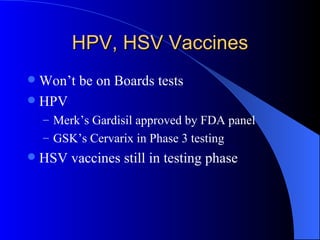
The document summarizes key points from a presentation on sexually transmitted diseases given at a 2007 conference. It covers various genital infections including herpes, syphilis, chlamydia, gonorrhea, bacterial vaginosis, trichomoniasis, human papillomavirus, and their signs, symptoms, diagnostic testing, and treatment recommendations. Resources on STD guidelines and management from the CDC are also referenced.