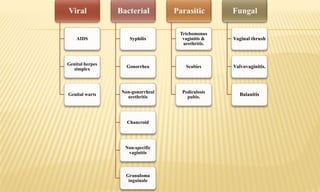
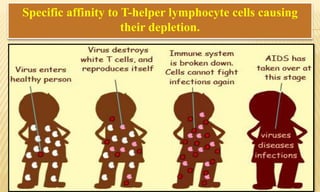
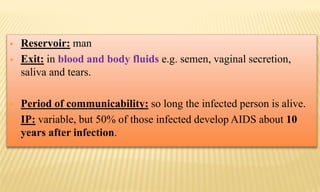
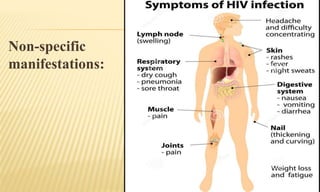
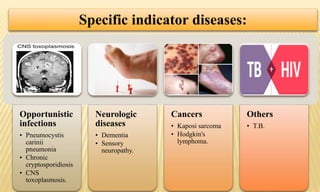
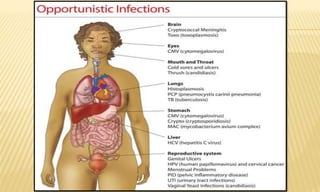
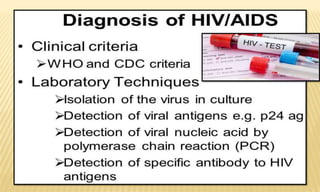
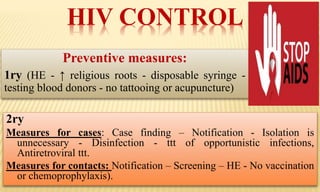
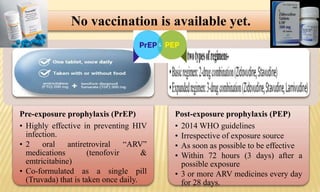
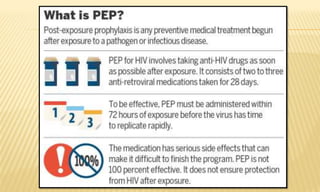
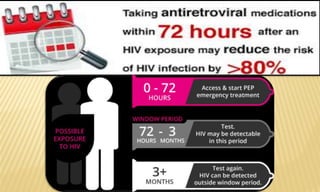
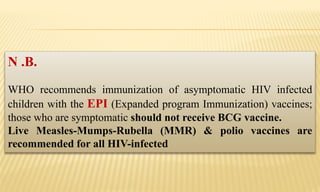
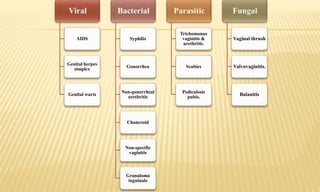
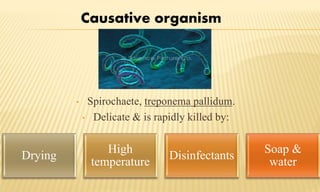
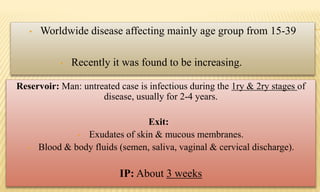
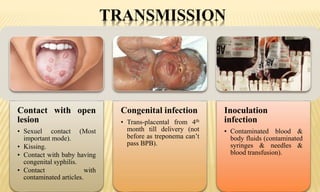
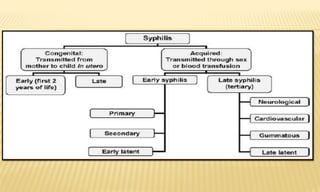
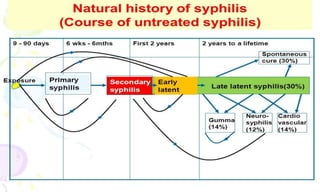
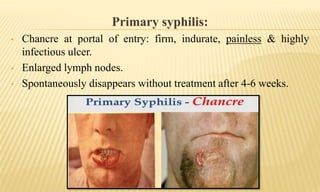
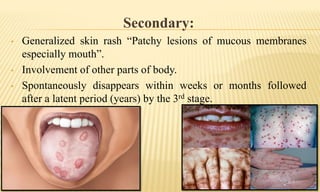
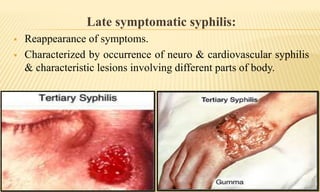
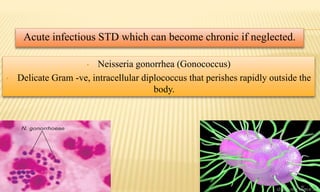
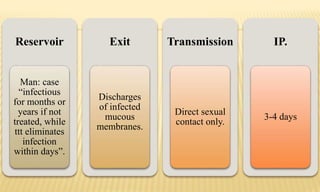
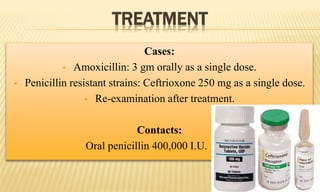
This document discusses sexually transmitted diseases (STDs), including AIDS, genital herpes, genital warts, syphilis, gonorrhea, and others. It provides details on causative agents, modes of transmission, clinical presentations, diagnosis, prevention, and treatment. STDs are a major public health issue due to their increasing worldwide incidence, high costs of treatment and complications, and their link to socioeconomic and behavioral factors.