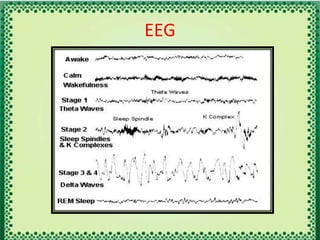
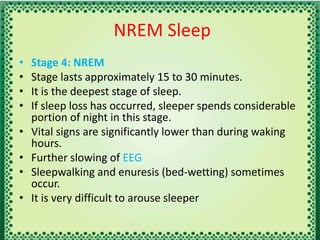
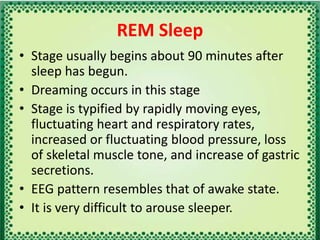
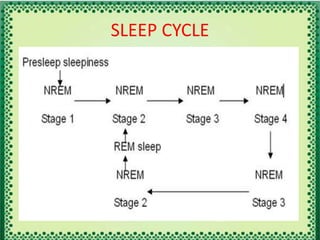
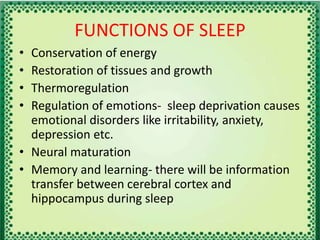
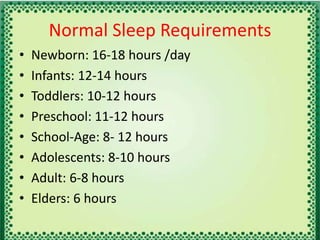
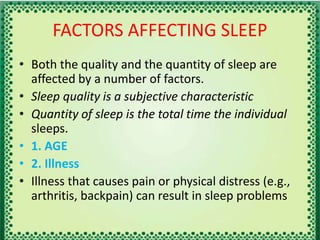
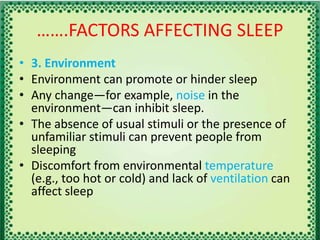
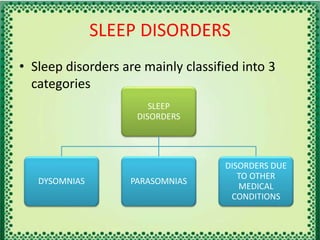
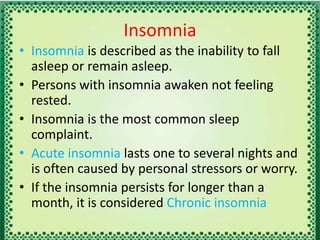
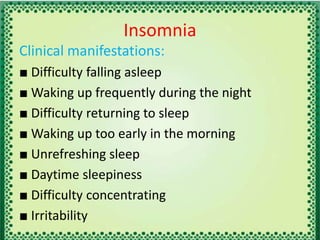
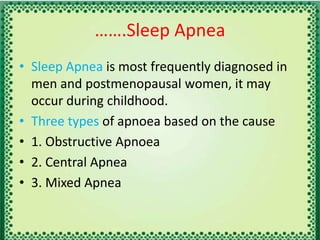
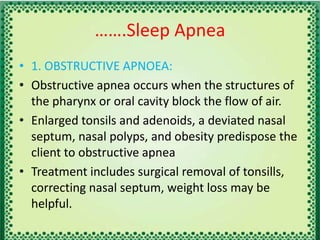
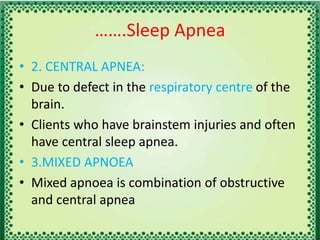
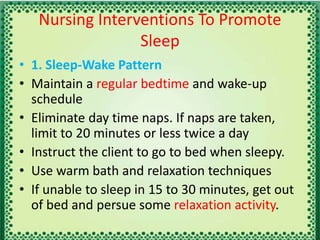
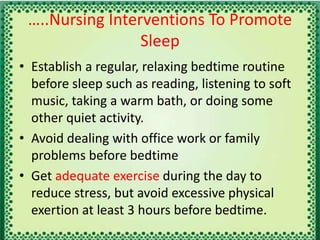
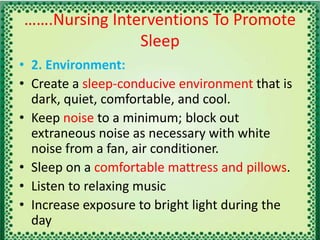
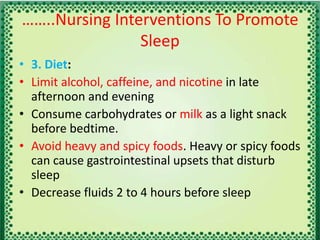
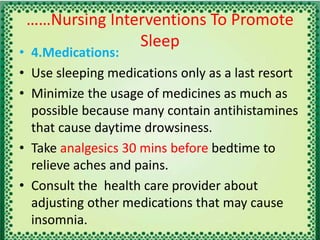
The document defines sleep and rest, explaining sleep as a state of rest characterized by altered consciousness and decreased perception, and outlines the physiological processes governing sleep, including the role of circadian rhythms and brain structures. It details stages of sleep, disorders such as insomnia and sleep apnea, and factors affecting sleep quality and quantity, alongside suggested nursing interventions for promoting better sleep. Overall, it covers the importance of sleep for physical and mental well-being and the impact of various lifestyle and environmental factors.