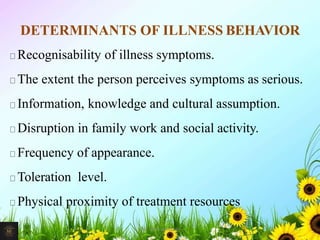
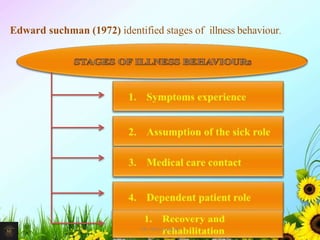
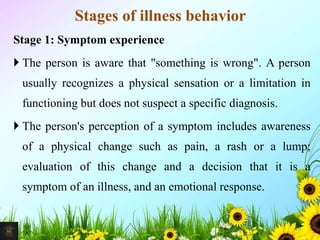
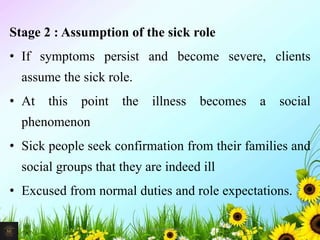
Illness can involve diminished physical, emotional, intellectual, social, or spiritual functioning compared to a person's previous experience. Risk factors for illness include genetics, age, environment, and lifestyle. Common causes of disease are biological agents, genetic defects, physical and chemical agents, tissue response to injury, metabolic processes, emotional stress, and medical treatment. Illness behavior is determined by factors such as symptom recognition, perceived severity, knowledge, and access to treatment resources. It progresses through stages from initial symptom experience to assuming a sick role to seeking medical care to dependent patient role to recovery.