The document discusses various topics related to sleep including:
1. Sleep accounts for about 1/3 of our lifetime and 1/3 of the population has a sleep disorder.
2. Sleep is regulated by our circadian rhythm located in the hypothalamus and lasts approximately 24 hours.
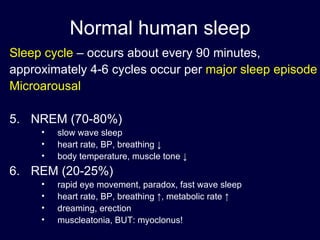
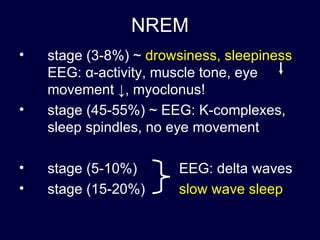
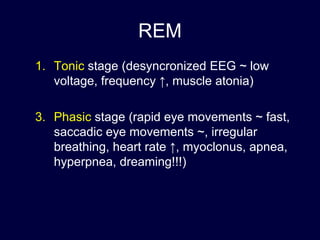
3. A normal sleep cycle occurs every 90 minutes and includes NREM sleep, which accounts for 70-80% of sleep, and REM sleep, which accounts for 20-25% of sleep.
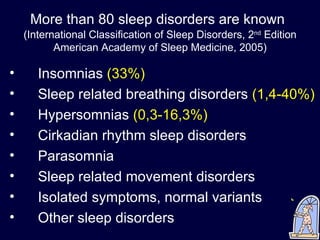
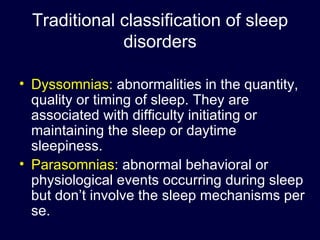
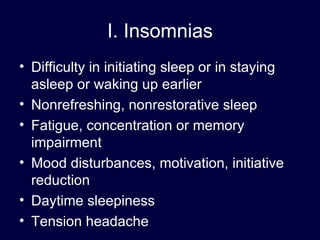
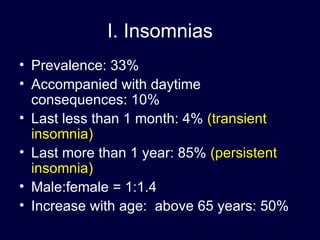
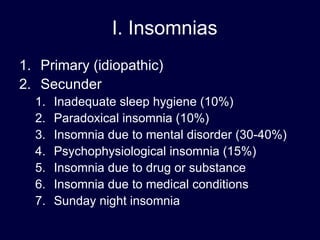
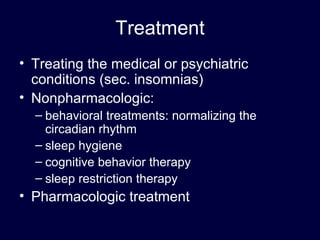
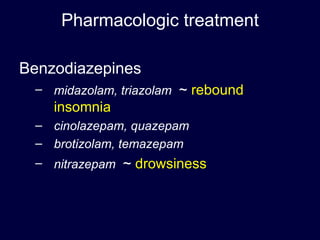
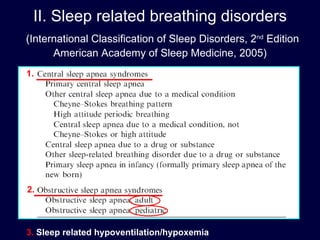
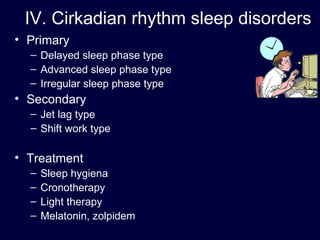
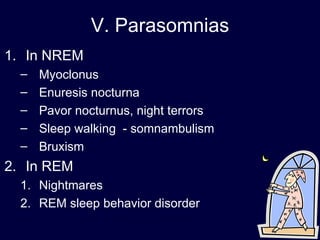
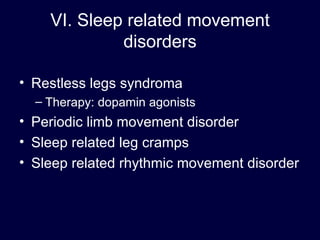
4. More than 80 known sleep disorders are classified as dyssomnias involving difficulties initiating or maintaining sleep or daytime sleepiness, or parasomnias involving abnormal events during sleep.