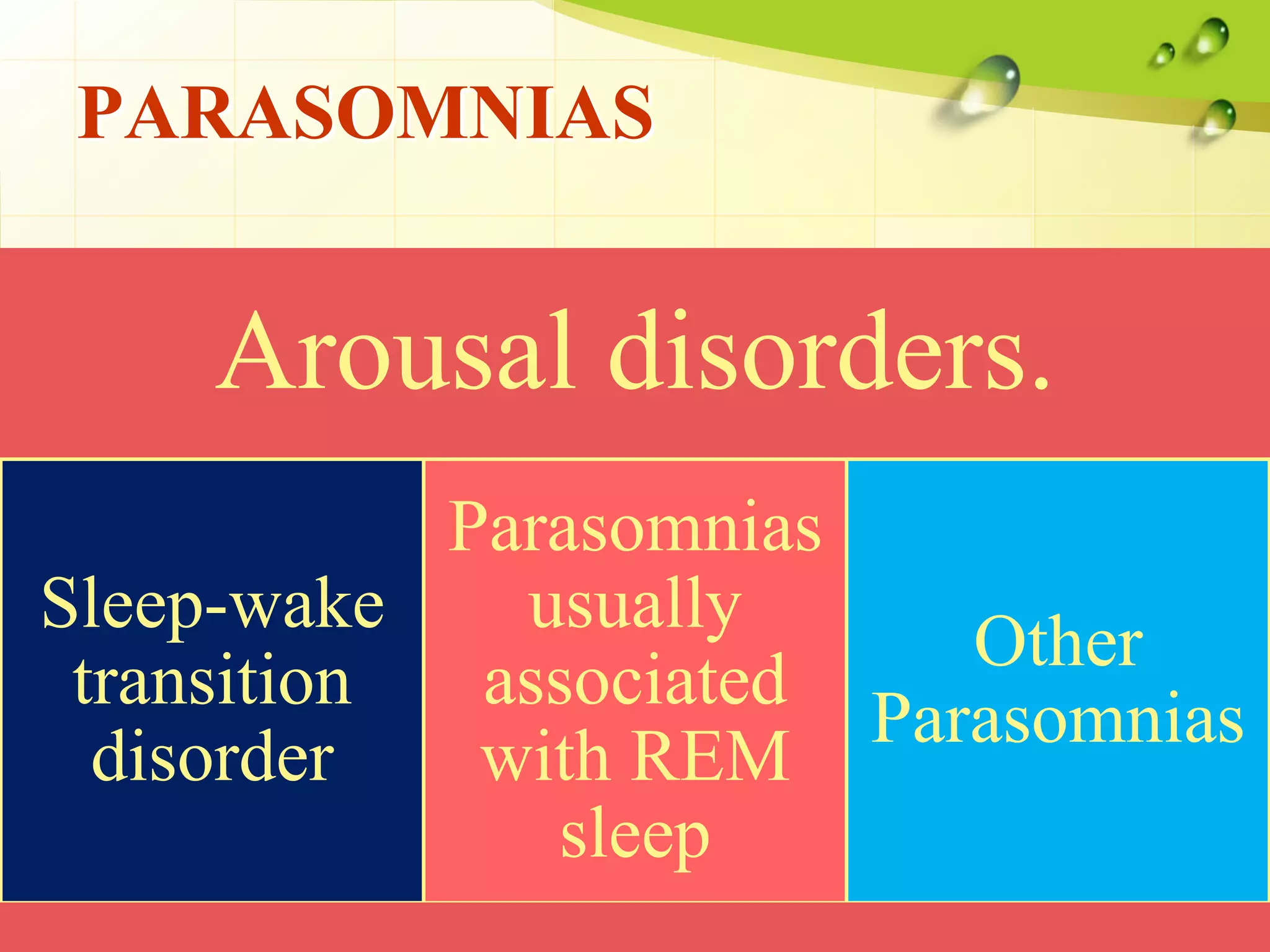
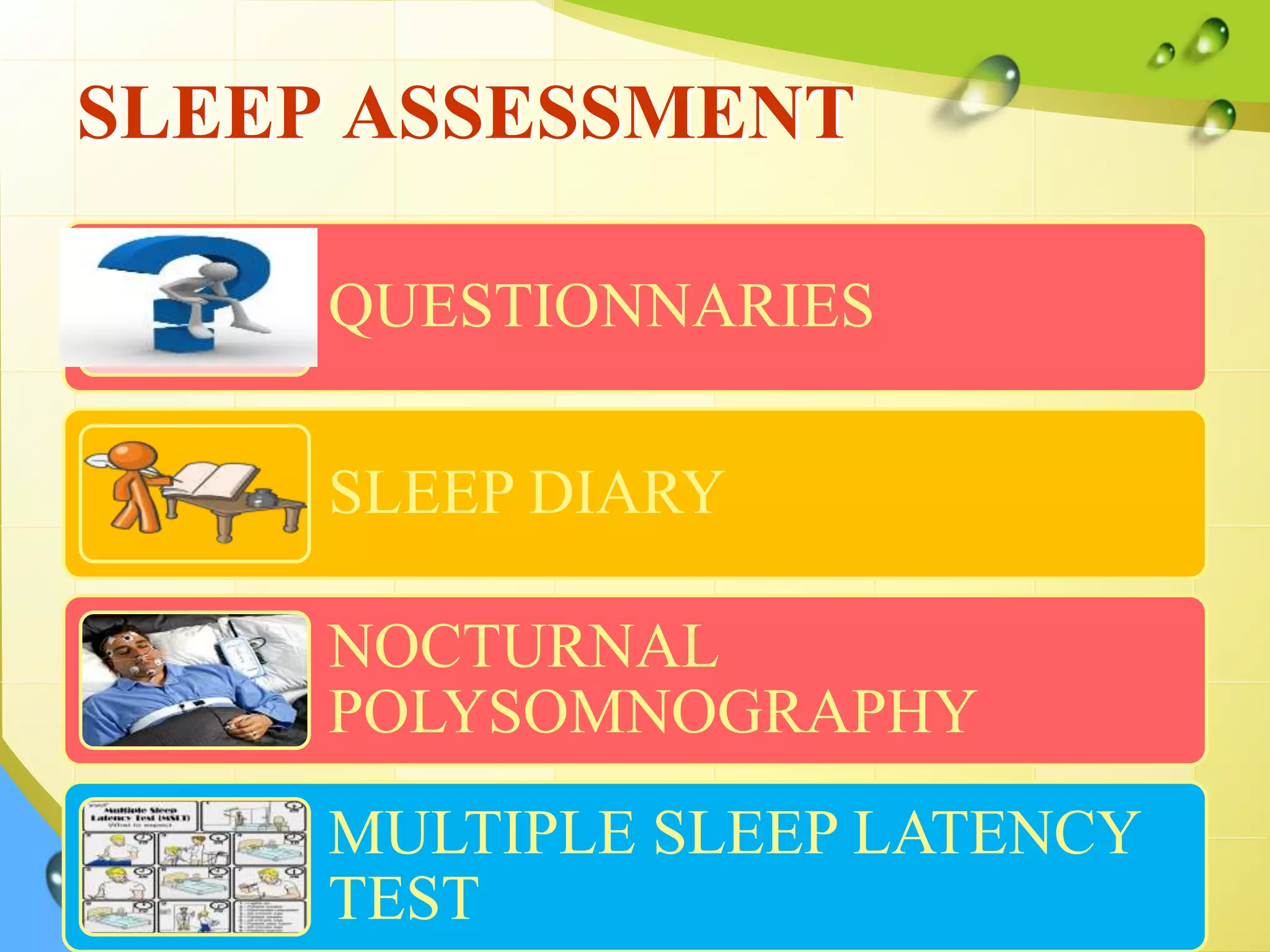
The document discusses sleep patterns, disturbances, and pain management, highlighting the physiological processes of sleep, stages of sleep, and the impact of age and other factors on sleep needs. It further explores various sleep disorders, including dyssomnias and parasomnias, and provides a detailed overview of pain as a sensory and emotional experience, encompassing its types, dimensions, and management strategies. Non-pharmacological and pharmacological therapies for pain relief, including TENS, acupuncture, and opioid analgesics, are also addressed.