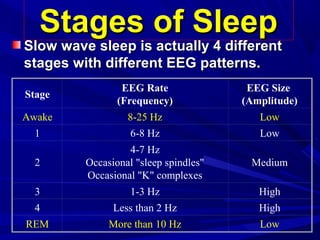
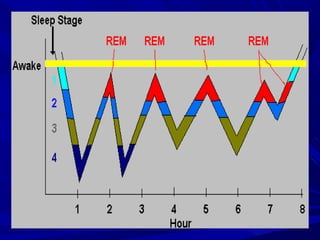
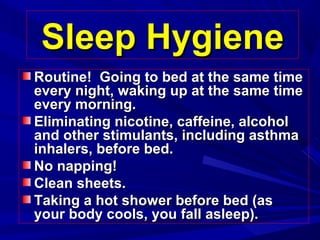
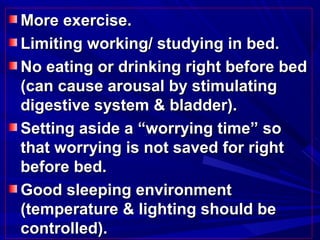
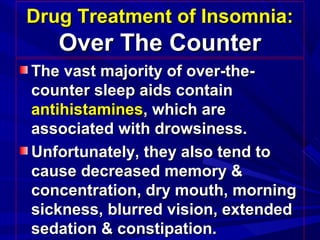
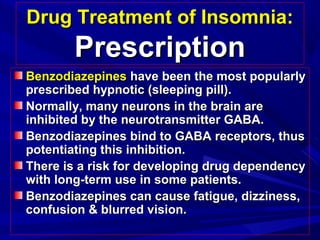
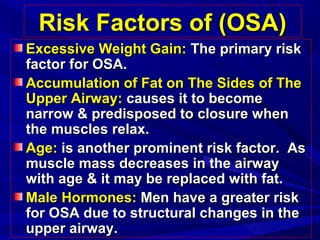
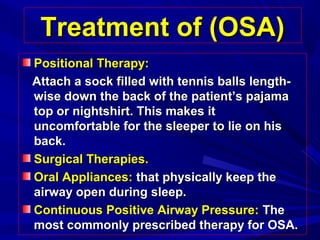
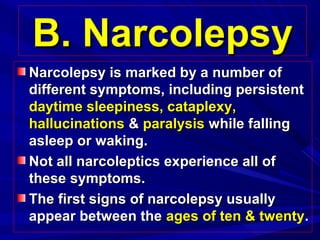
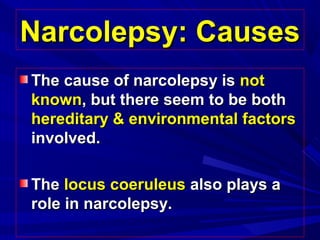
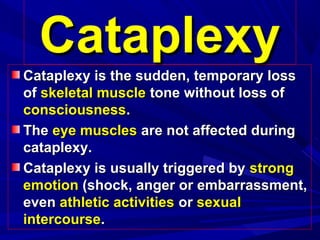
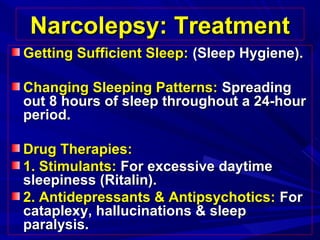
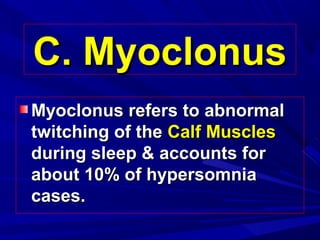
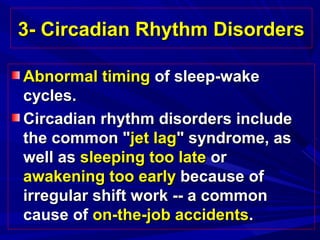
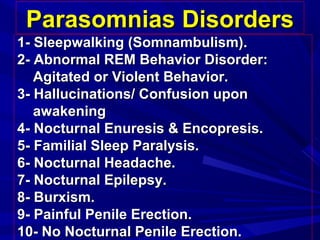
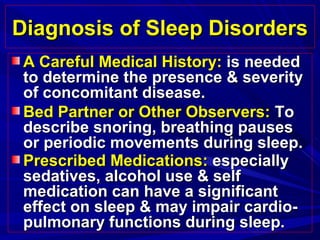
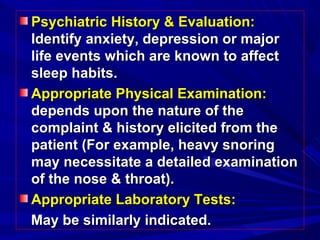
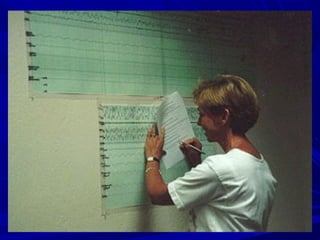
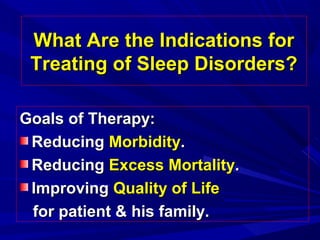
This document discusses sleep disorders, their causes, symptoms, diagnosis, and treatment. It covers several types of sleep disorders including insomnia, hypersomnia, circadian rhythm disorders, and parasomnias. Insomnia is difficulty falling or staying asleep and can be acute or chronic. Hypersomnia involves excessive daytime sleepiness and is often caused by sleep apnea, narcolepsy, or myoclonus. Circadian rhythm disorders disrupt normal sleep-wake cycles. Parasomnias distort normal sleep architecture and include sleepwalking and REM behavior disorder. Diagnosis involves medical history, observation, exams, and tests. Treatment goals are reducing morbidity, mortality, and improving quality of life.