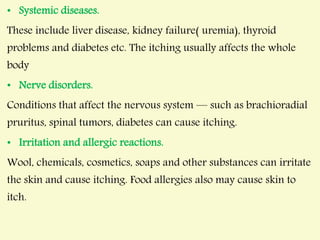
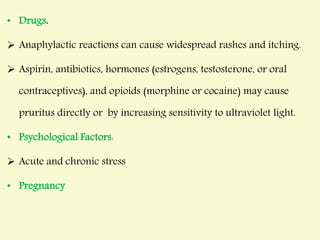
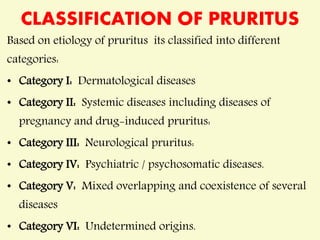
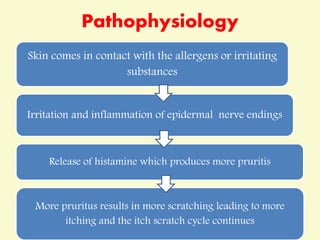
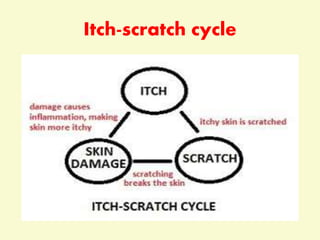
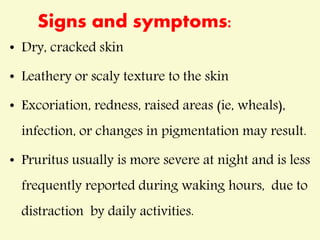
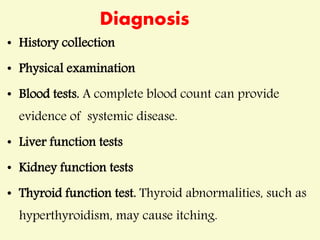
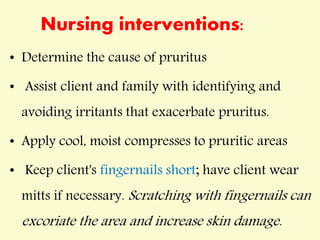
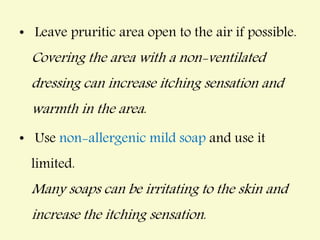
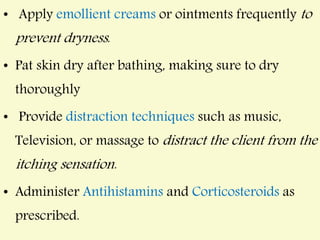
This document discusses pruritus (itching) by defining it, listing common causes such as dry skin, skin conditions, systemic diseases, nerve disorders, allergic reactions, drugs, and psychological factors. It describes the pathophysiology of the itch-scratch cycle and classification of pruritus. Diagnosis involves history, physical exam, and potential lab tests. Management includes topical corticosteroids, oral antihistamines, antidepressants, treating underlying causes, phototherapy, and nursing interventions like moisturizing and distraction techniques. Complications can be skin injury, infection, and scarring if scratching is not prevented.