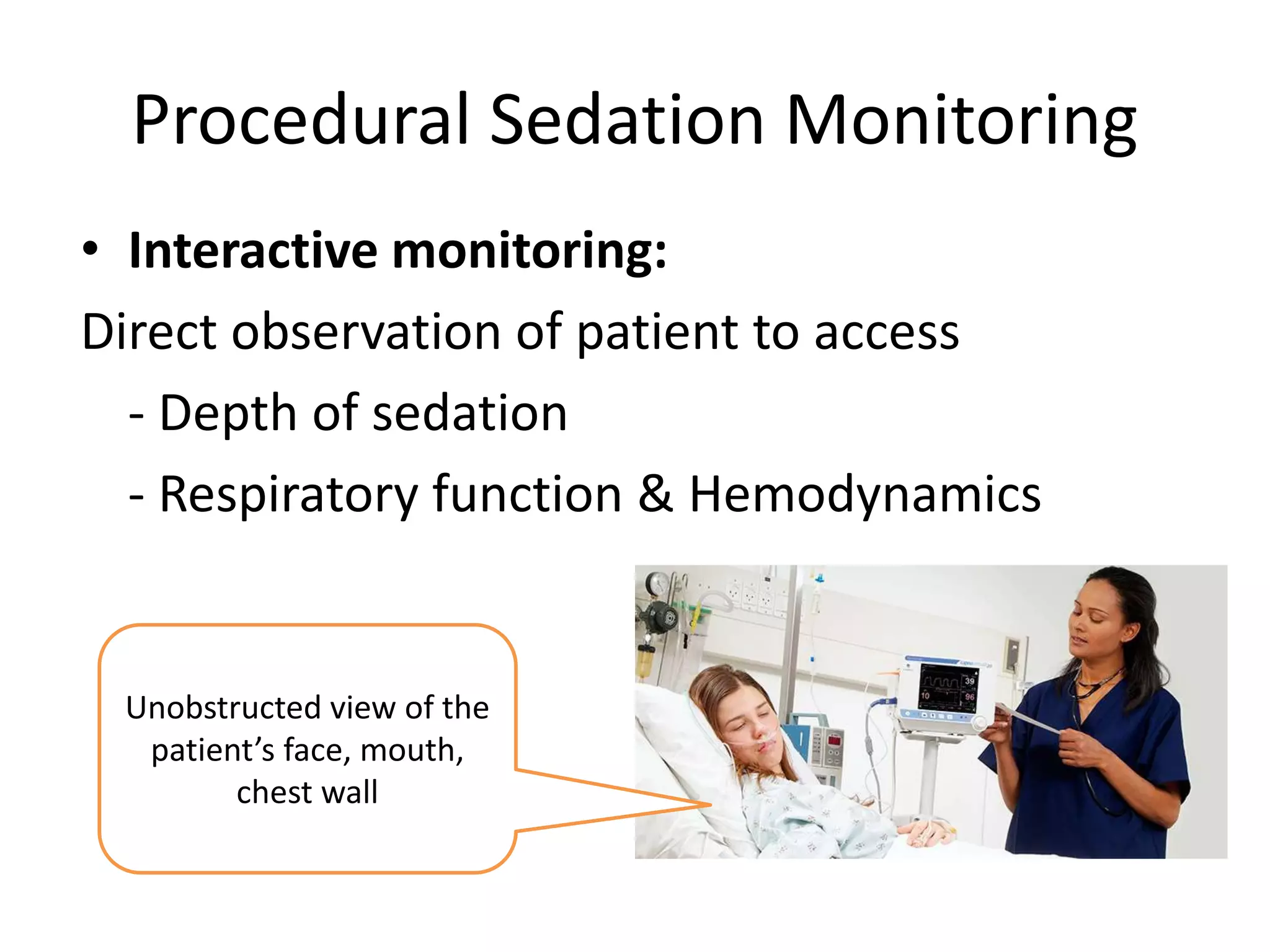
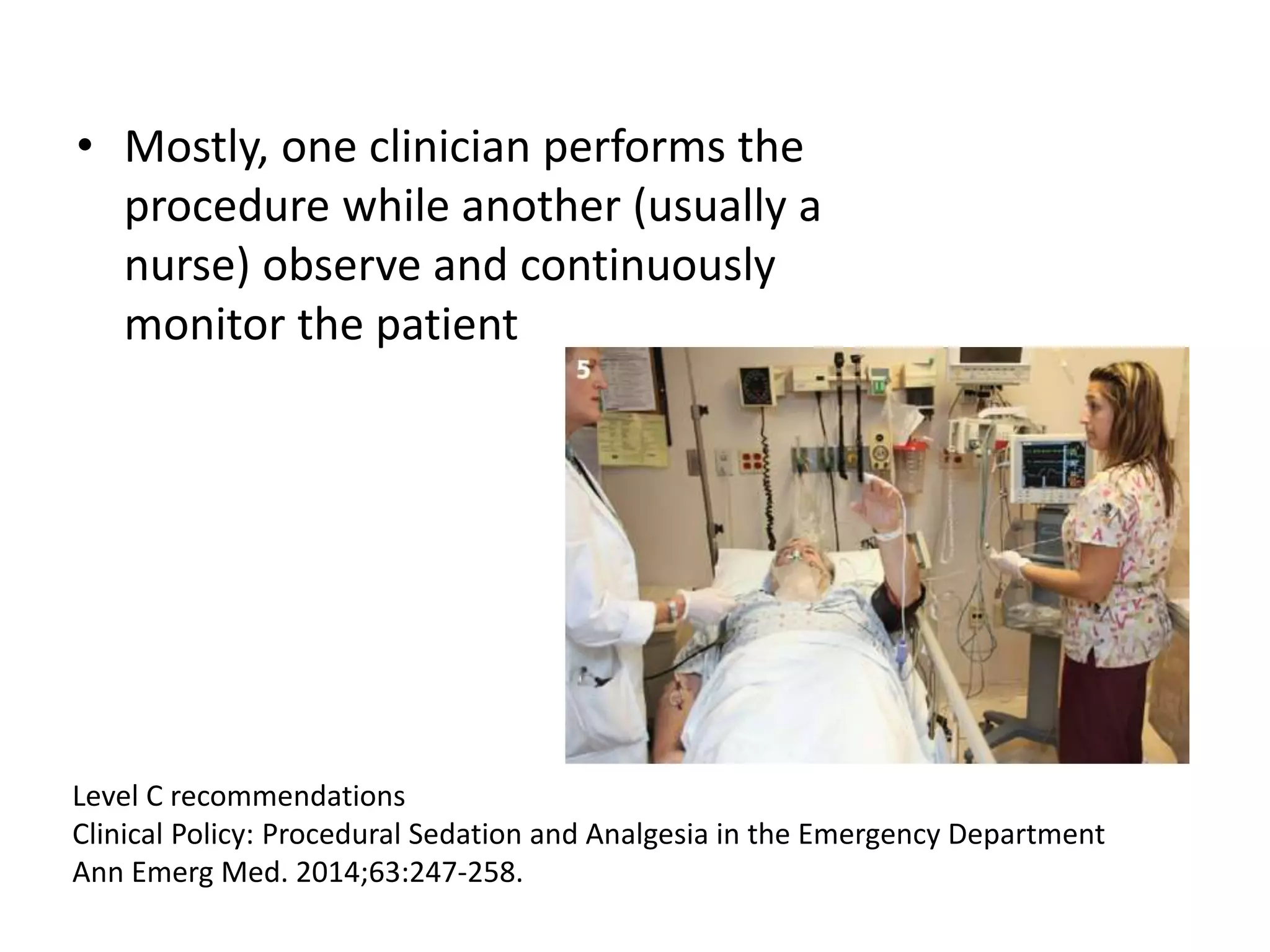
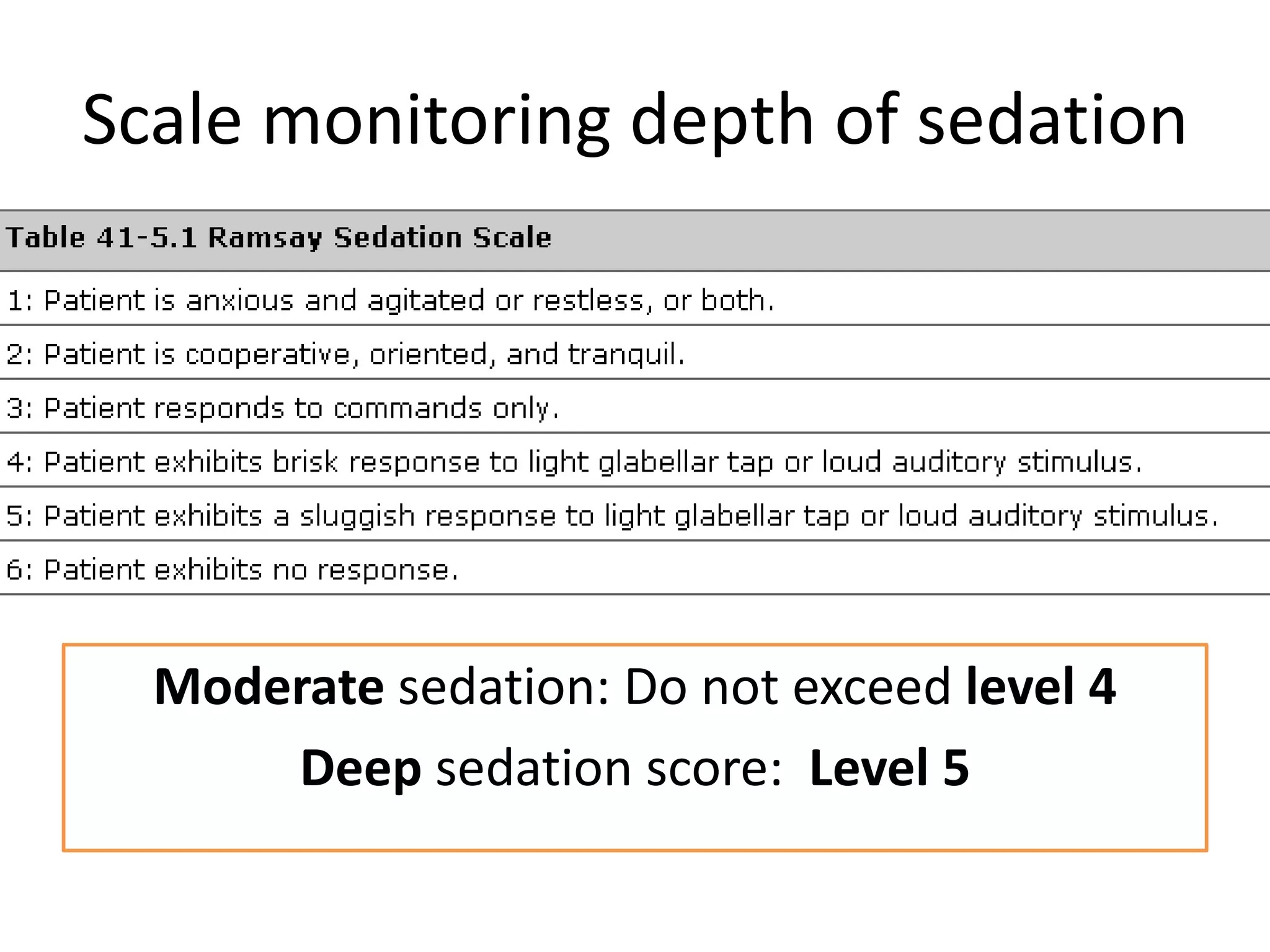
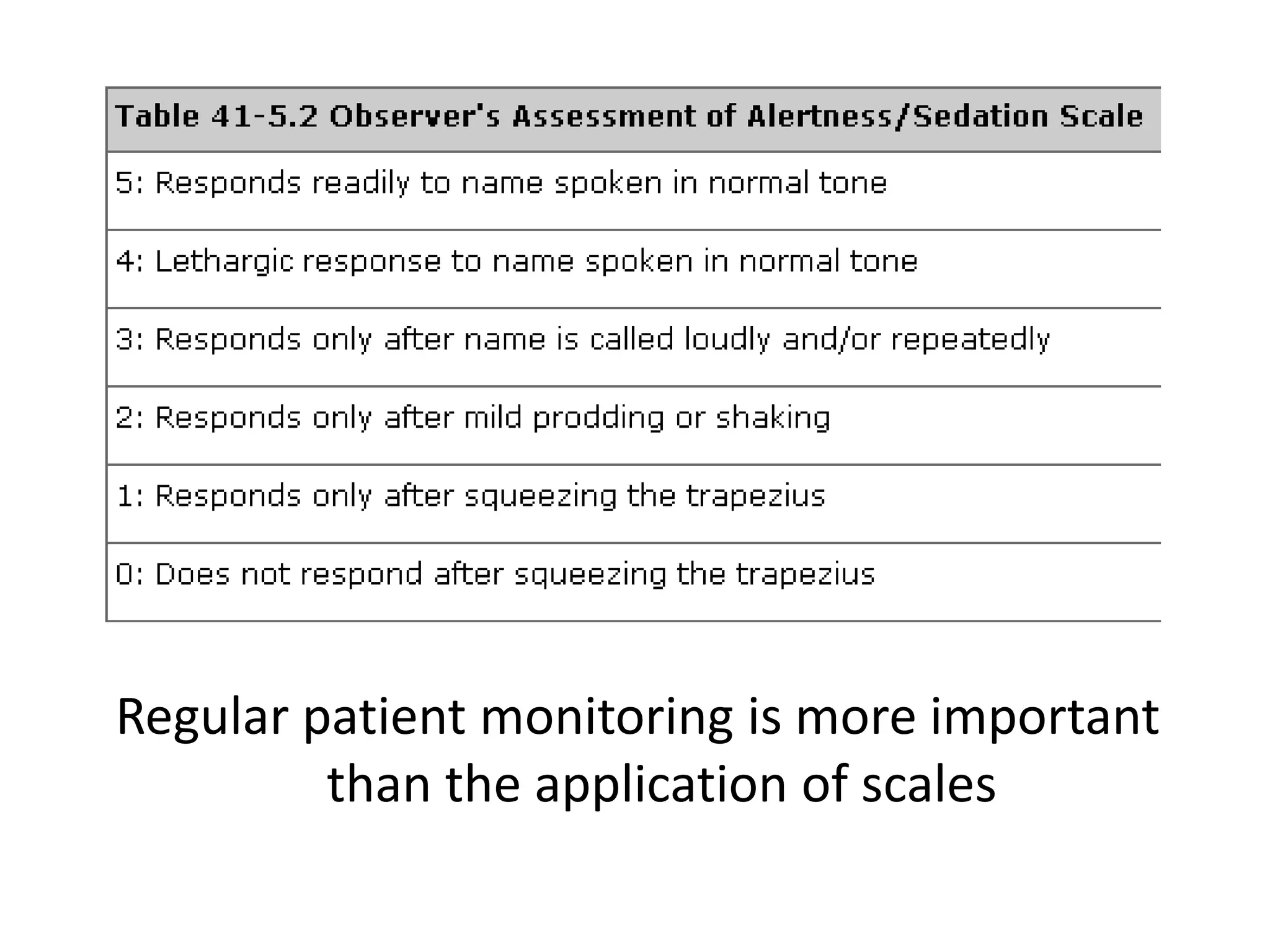
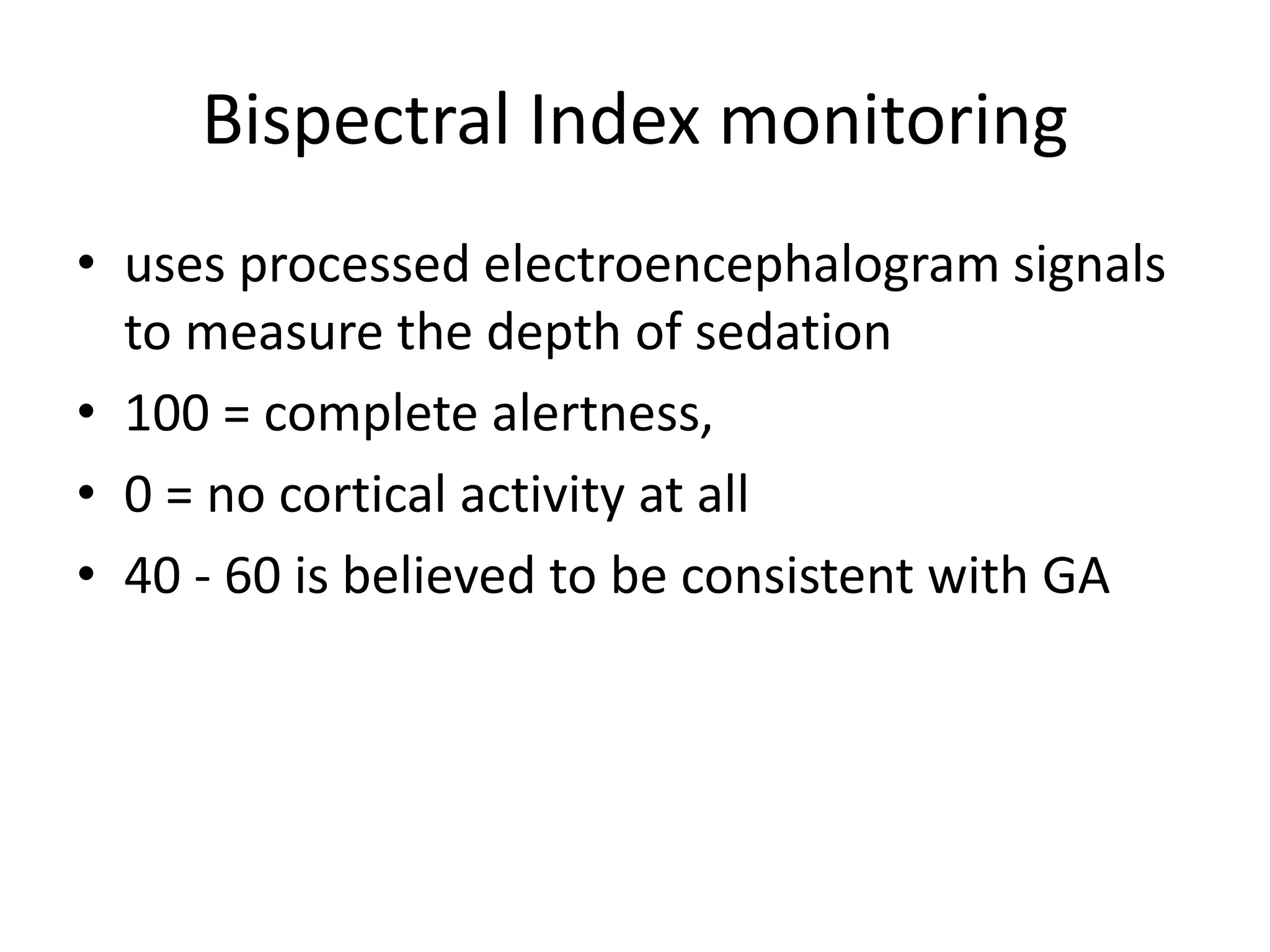
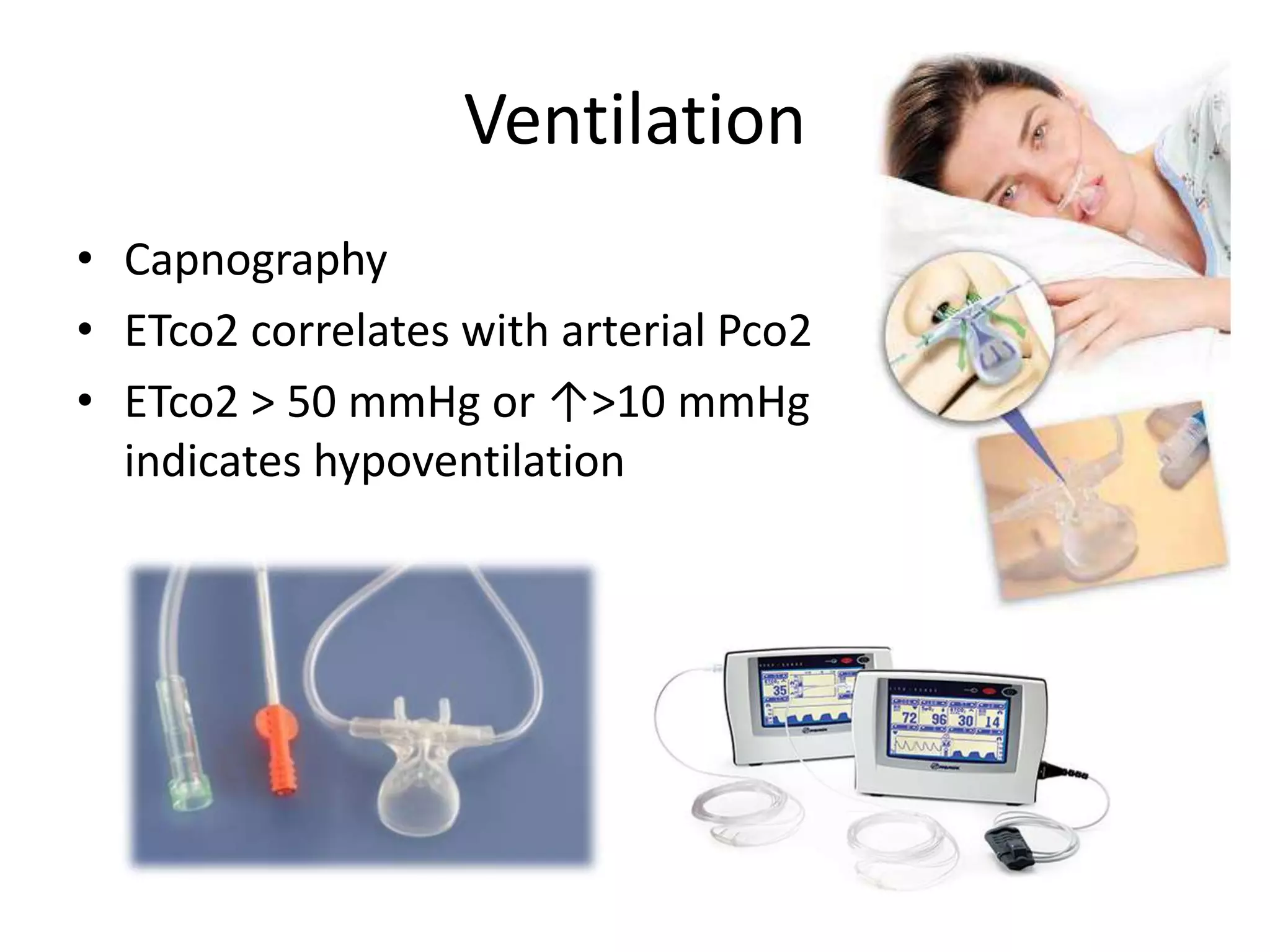
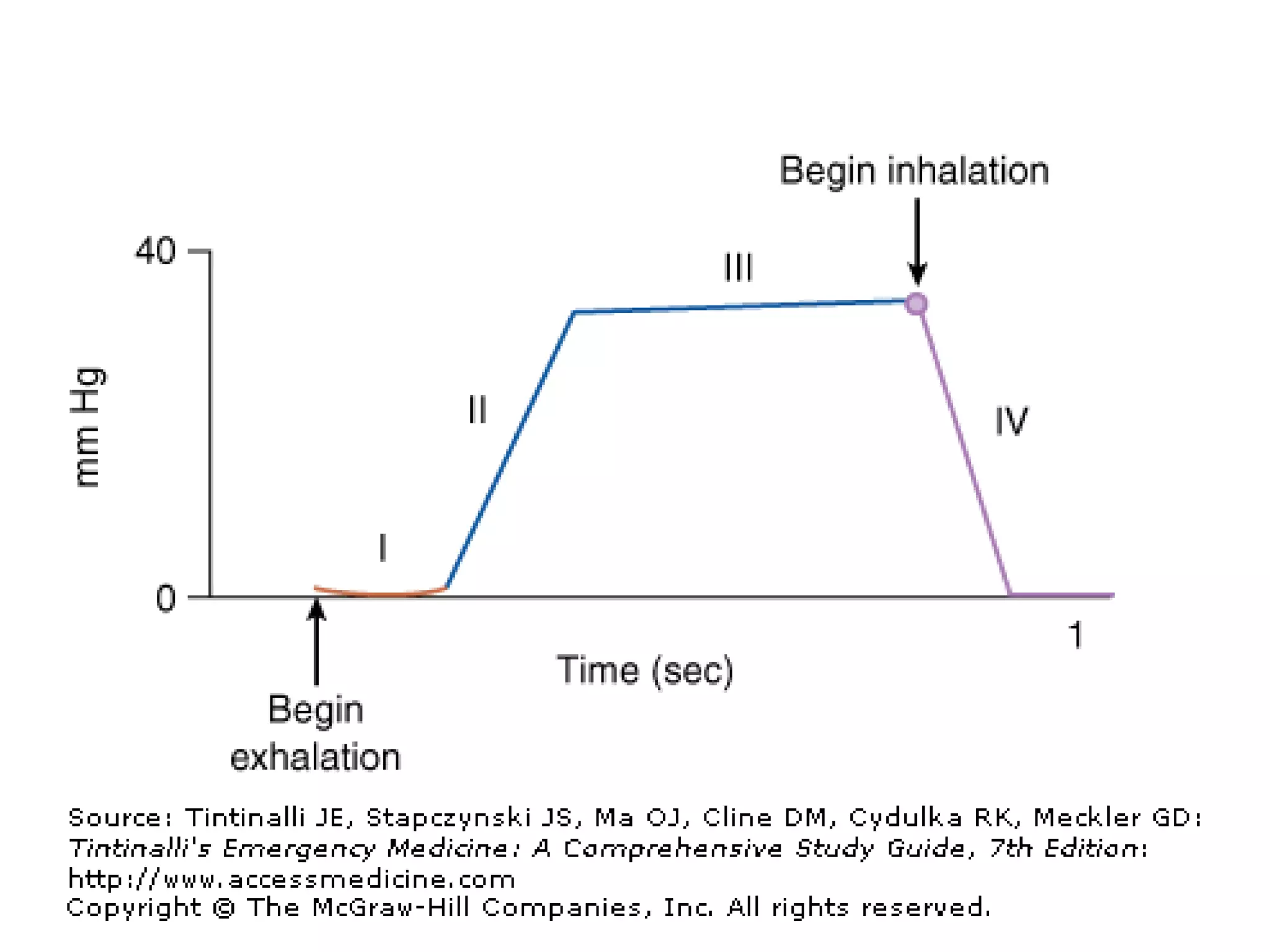
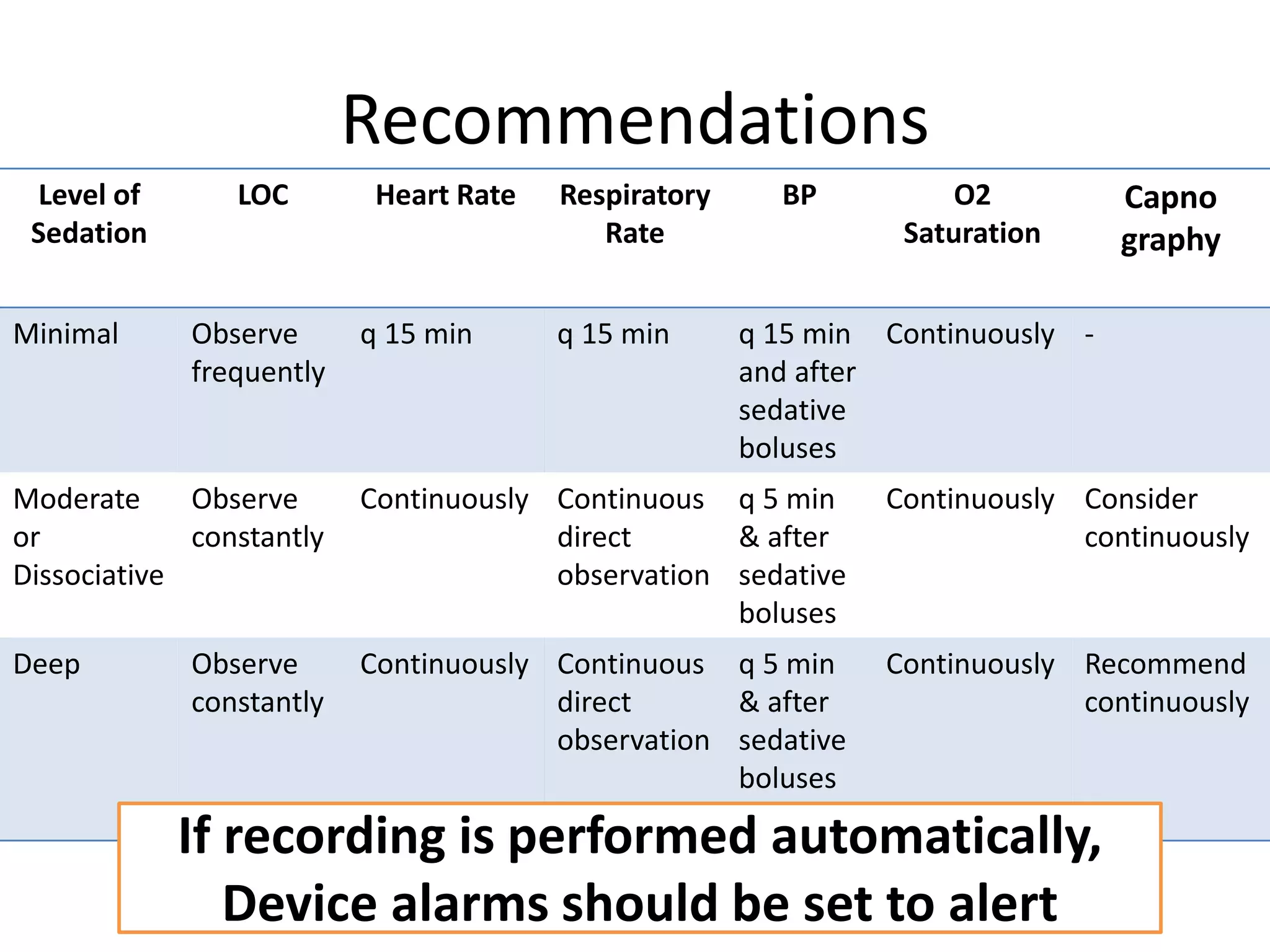
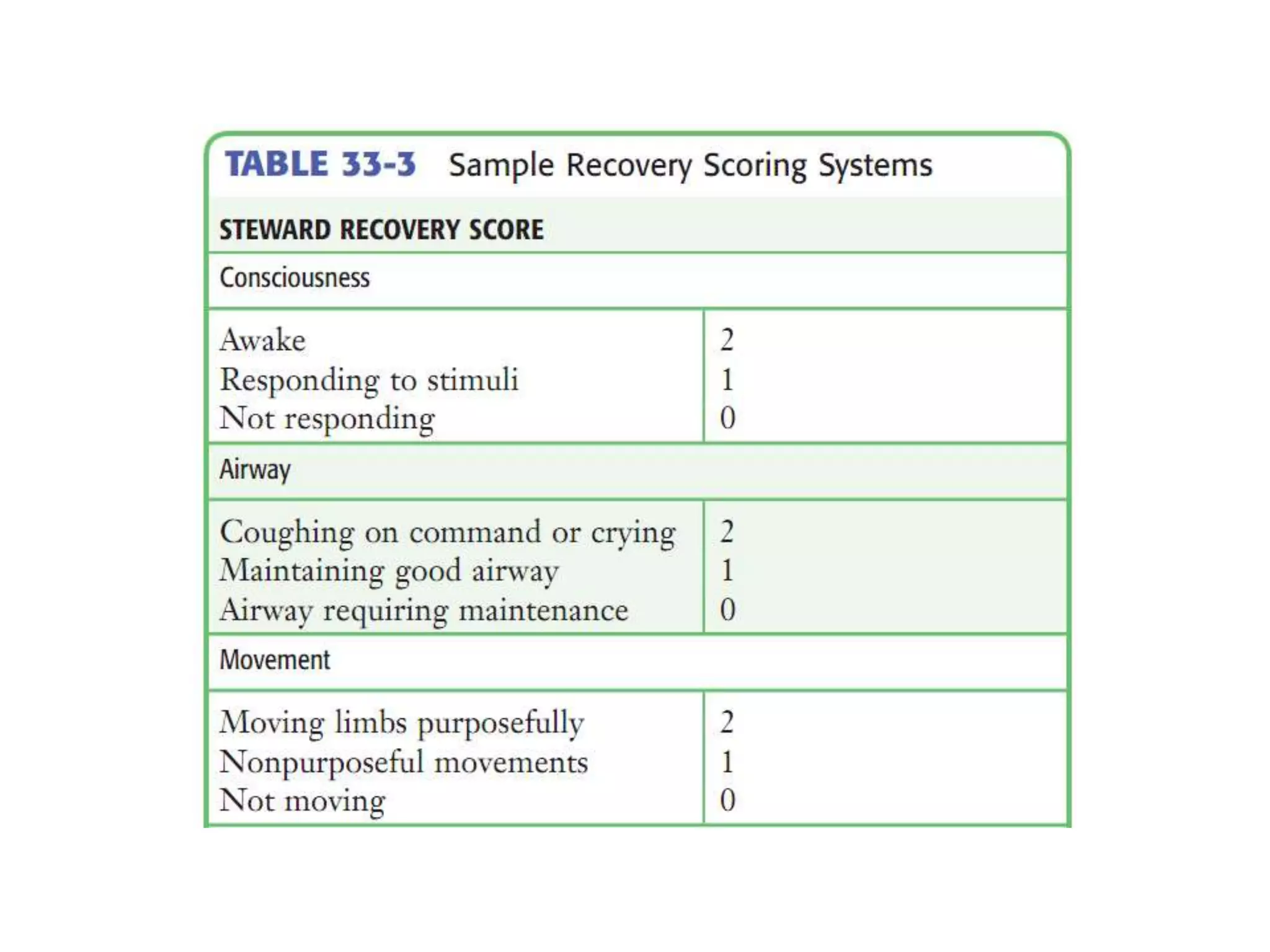
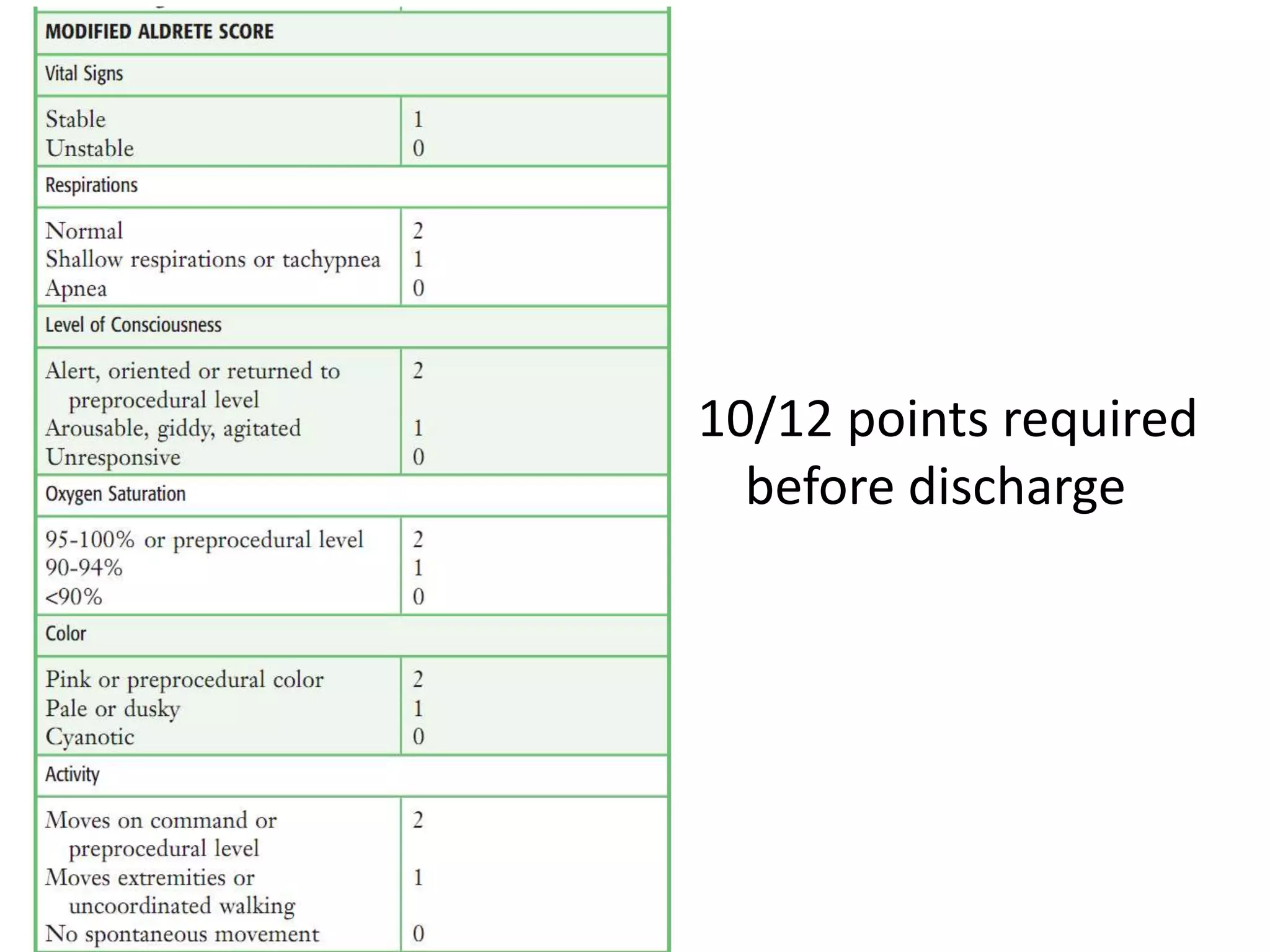
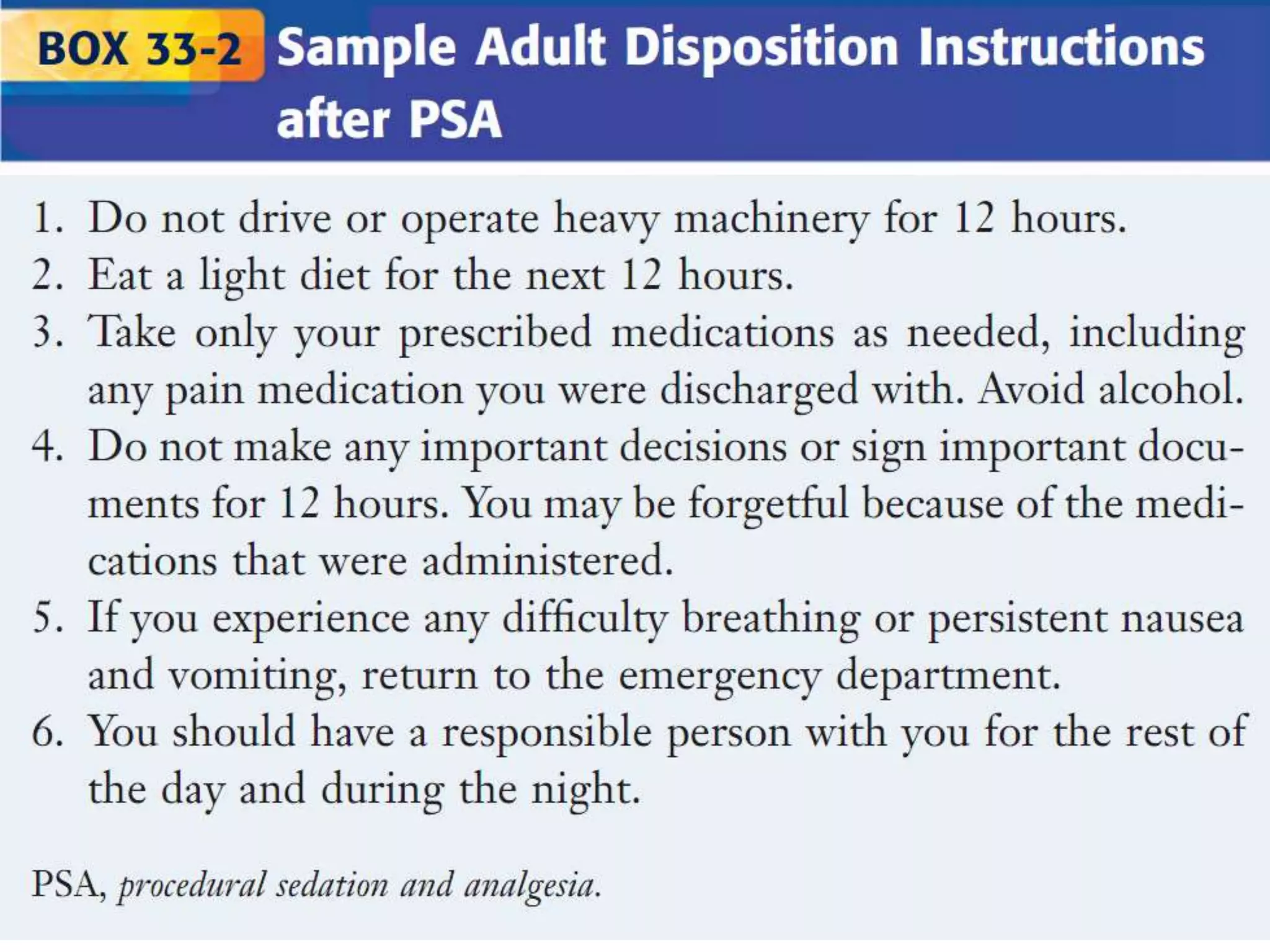
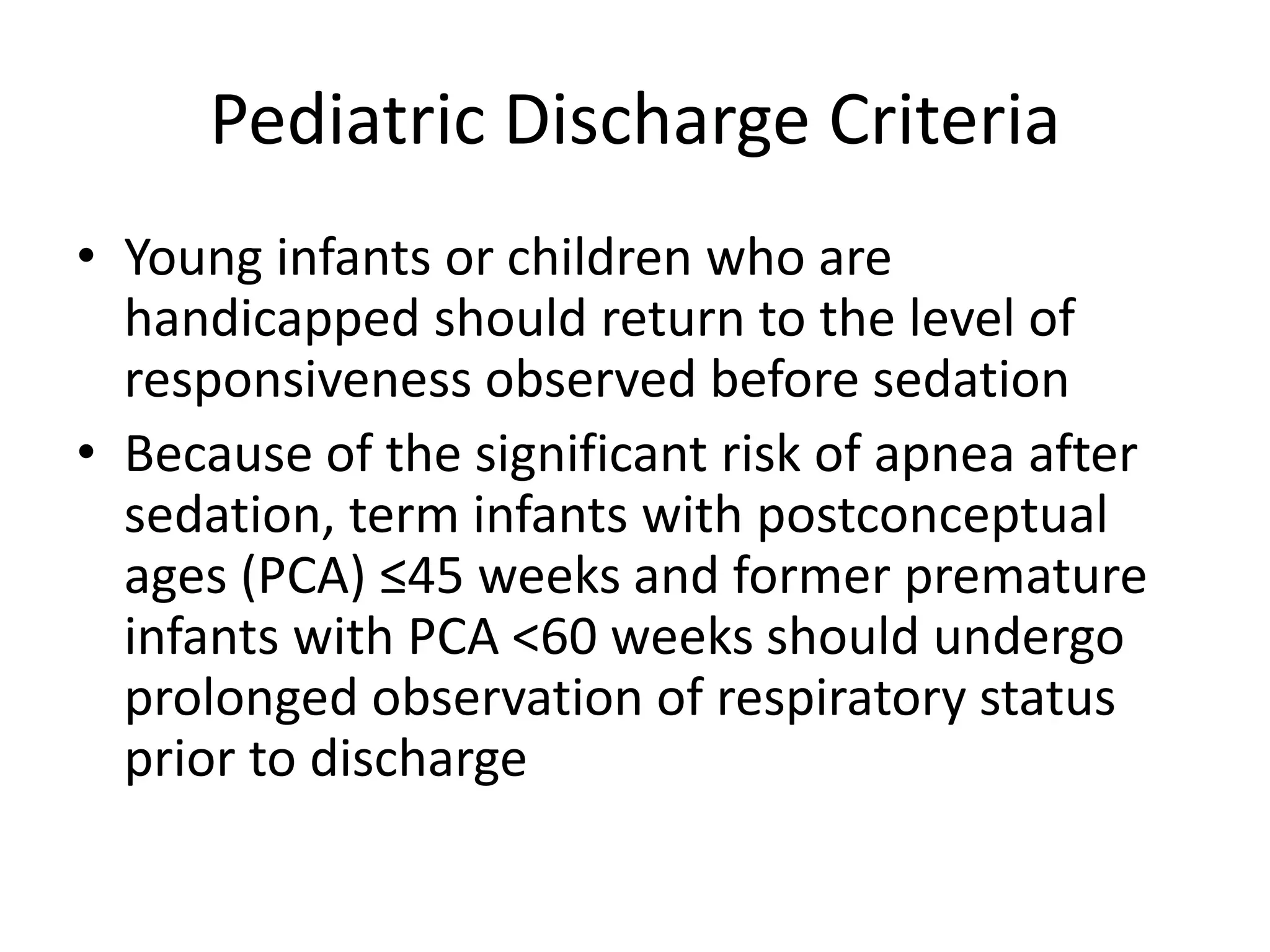
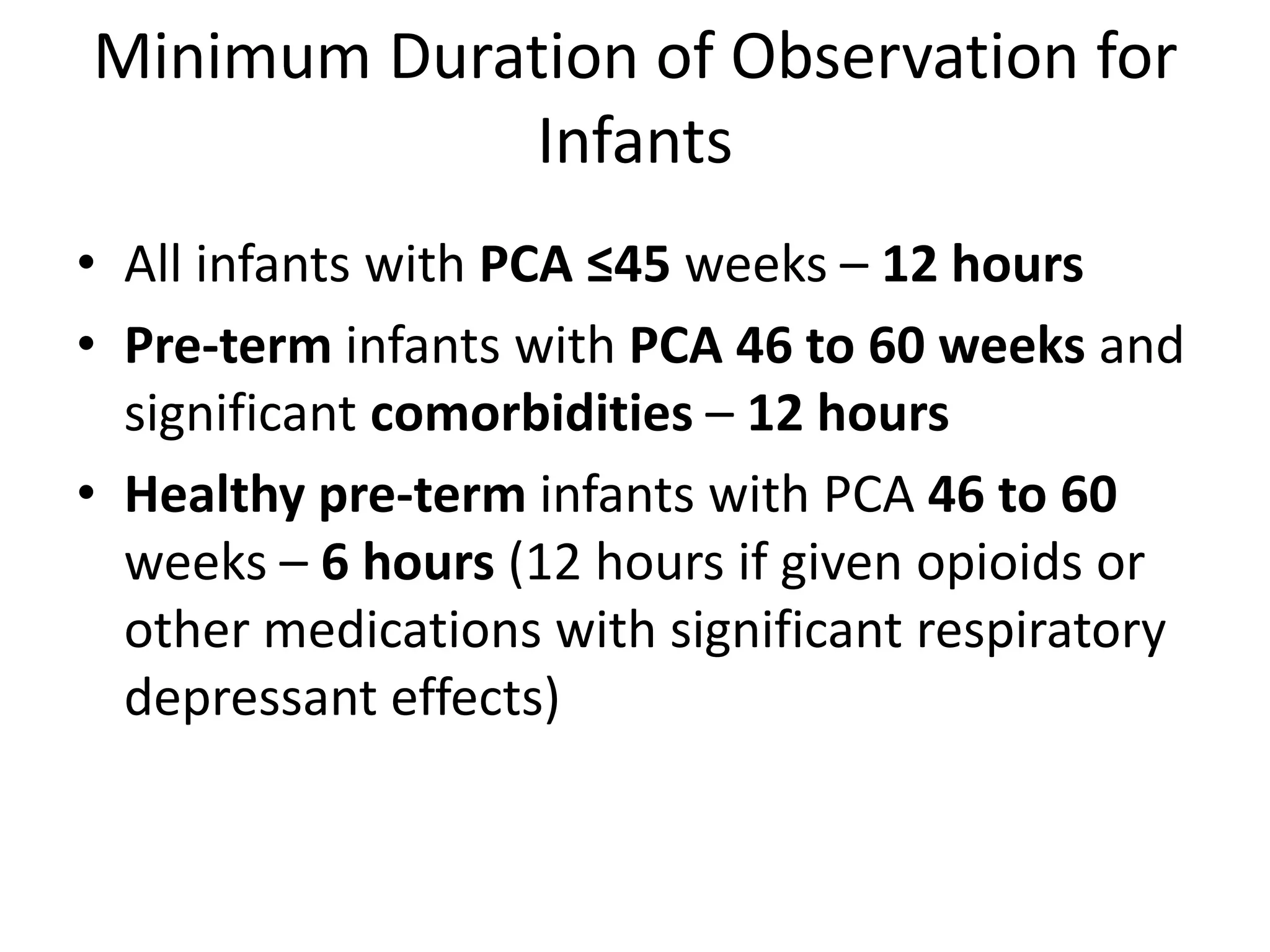
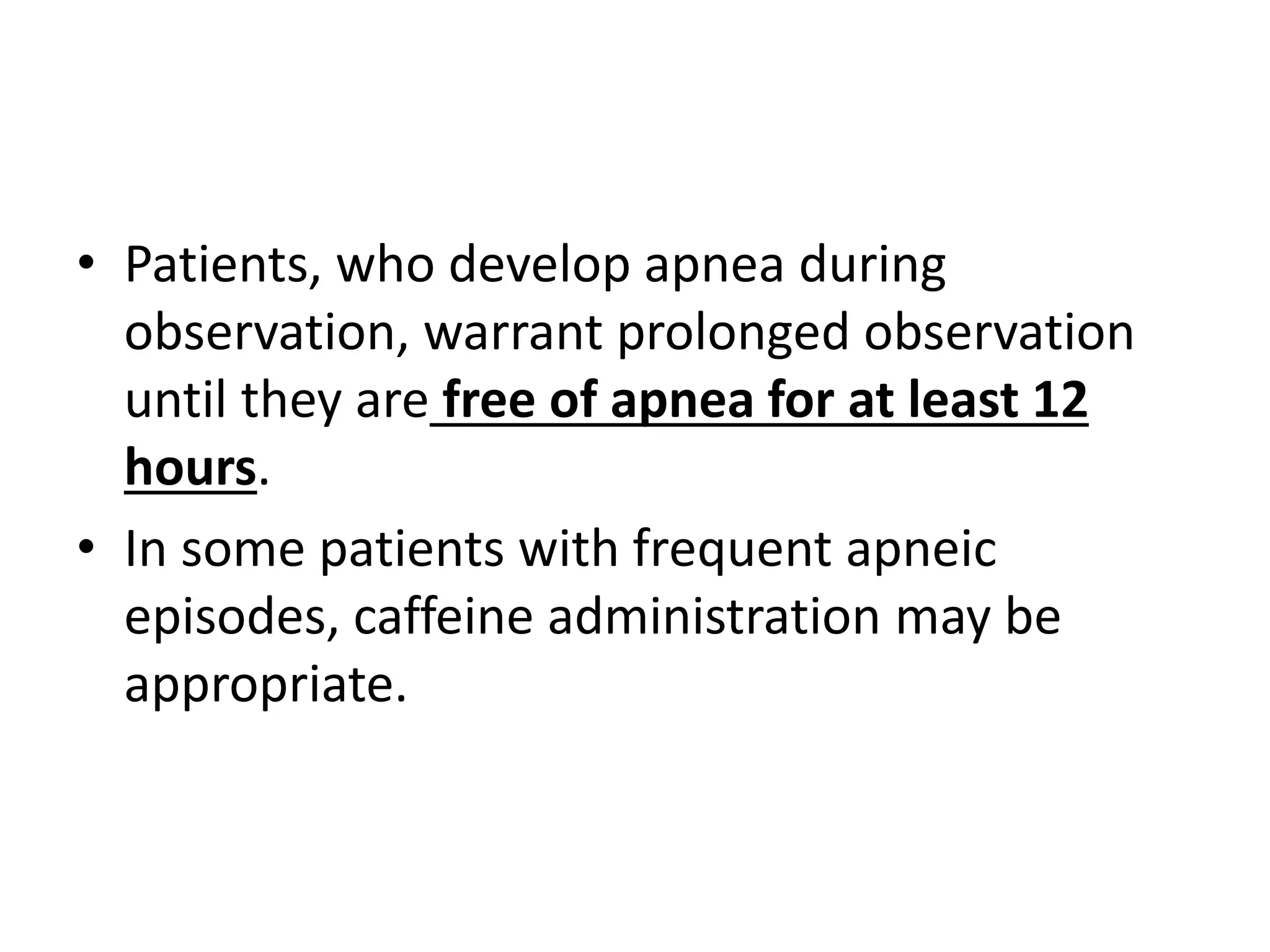
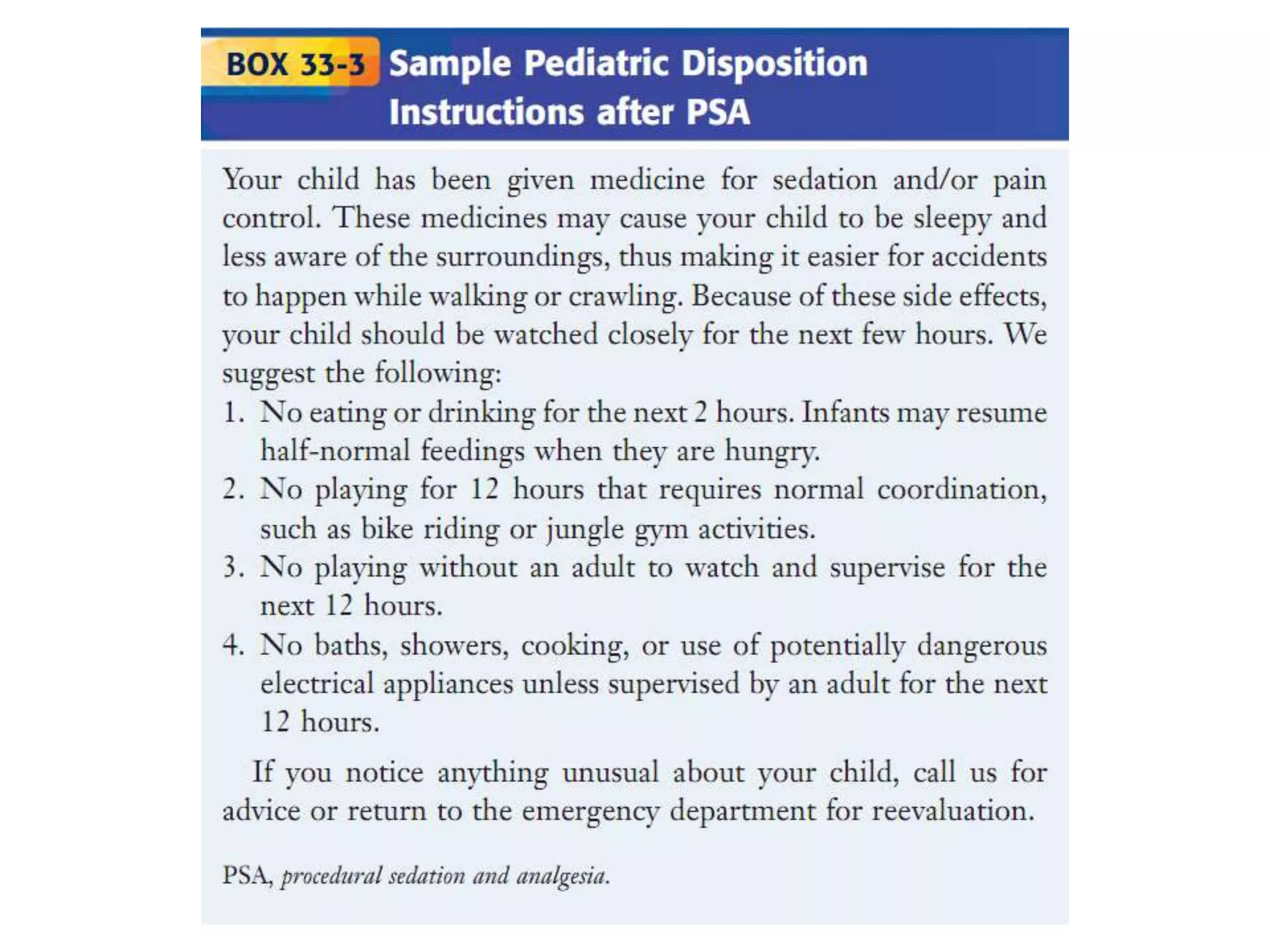
This document outlines guidelines for procedural sedation and analgesia. It recommends having appropriate monitoring equipment and administering analgesics before sedatives. Patients should be monitored until recovery to their baseline mental status. At minimum, procedural sedation requires one clinician to perform the procedure while another continuously monitors the patient. Regular monitoring of vital signs, oxygen saturation, and ventilation is important. The use of capnography may help detect respiratory complications earlier than pulse oximetry alone. Patients must meet discharge criteria related to symptoms, vital signs, and orientation before being discharged.