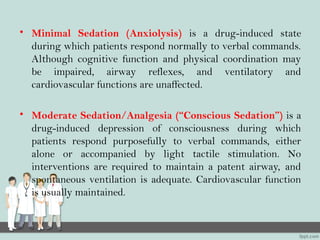
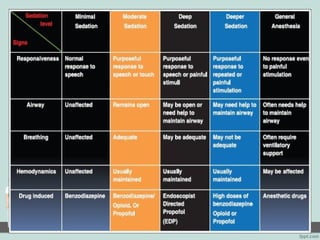
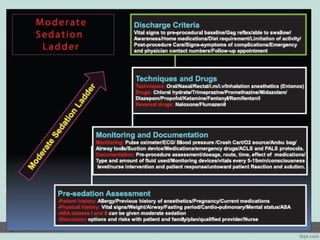
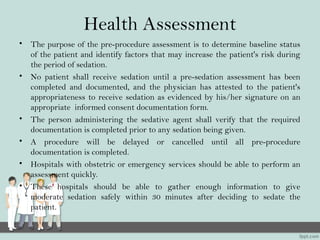
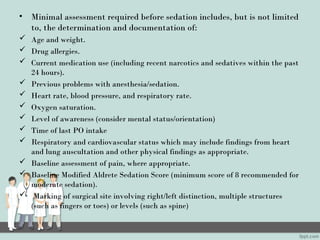
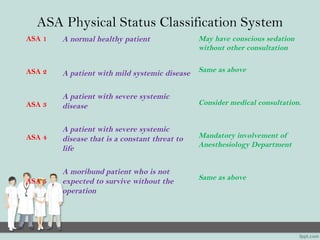
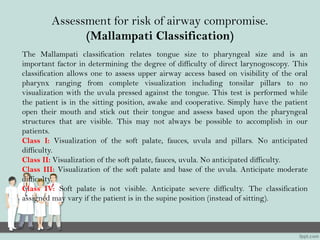
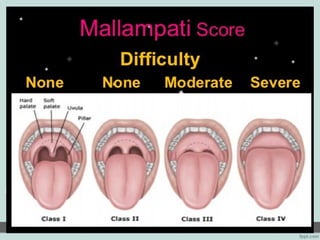
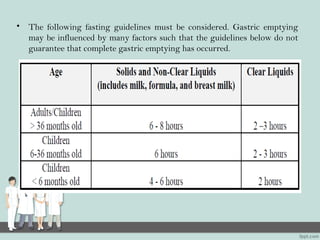
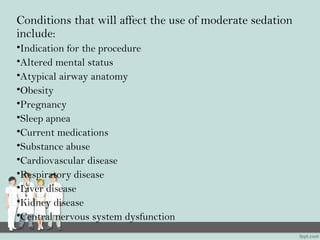
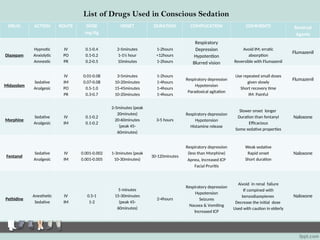
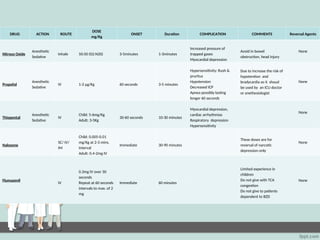
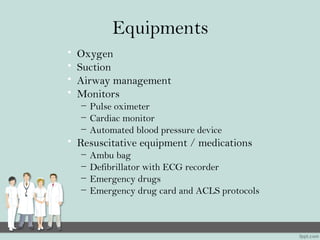
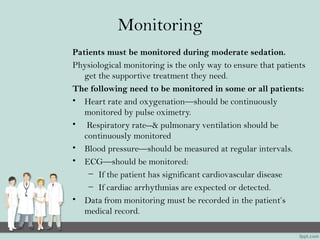
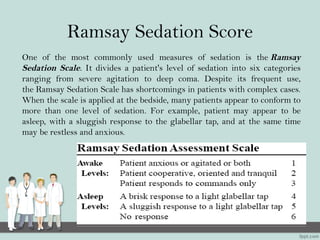
The document outlines the guidelines and standards for procedural sedation within hospitals, emphasizing the importance of uniform administration, qualified staff, and patient safety. It details pre-assessment requirements, monitoring protocols, and documentation necessary before, during, and after sedation, ensuring informed consent and addressing potential risks. The document also covers the various depths of sedation, sedation agents, and the responsibilities of healthcare providers in managing patient care during sedation procedures.