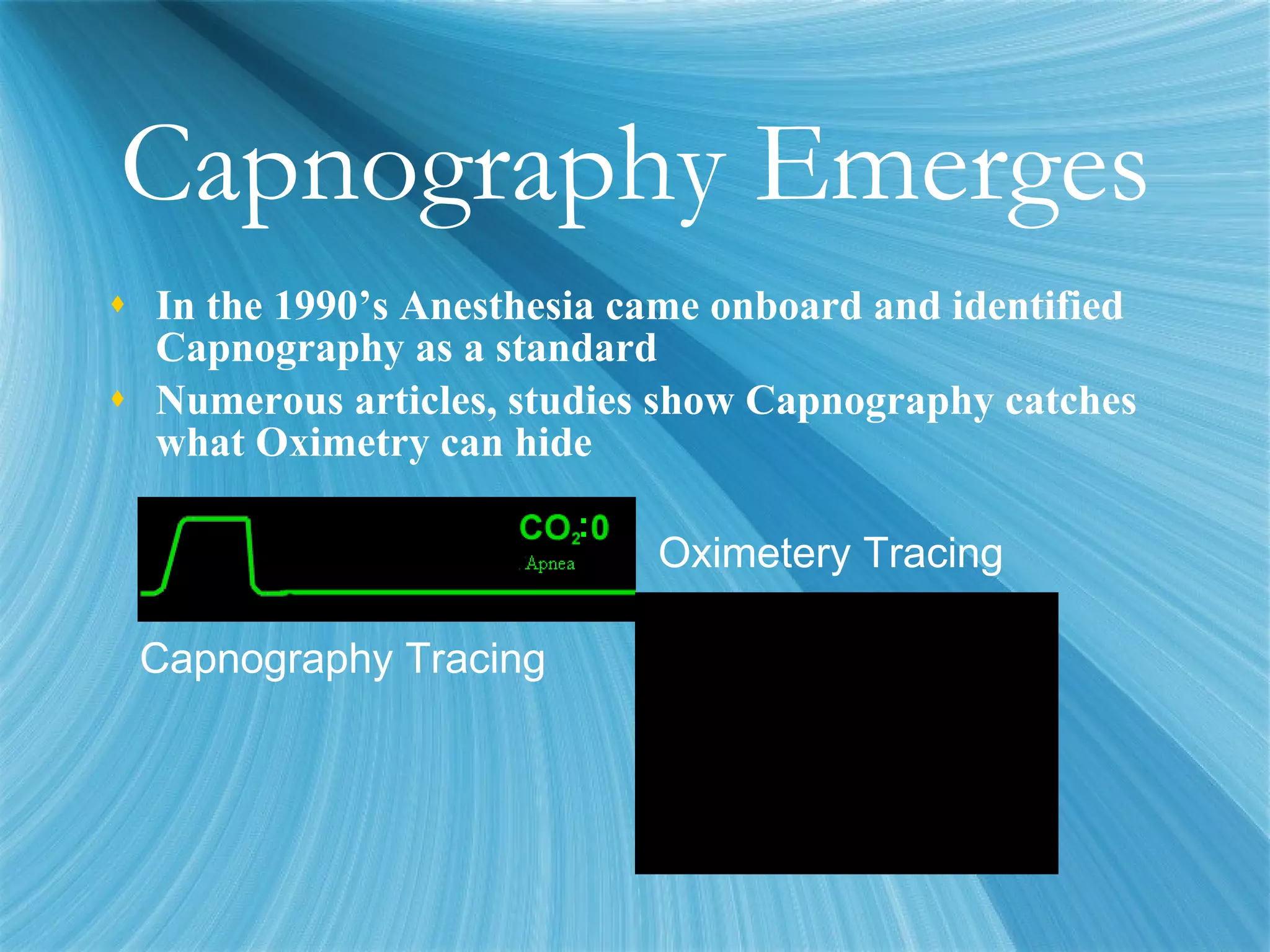
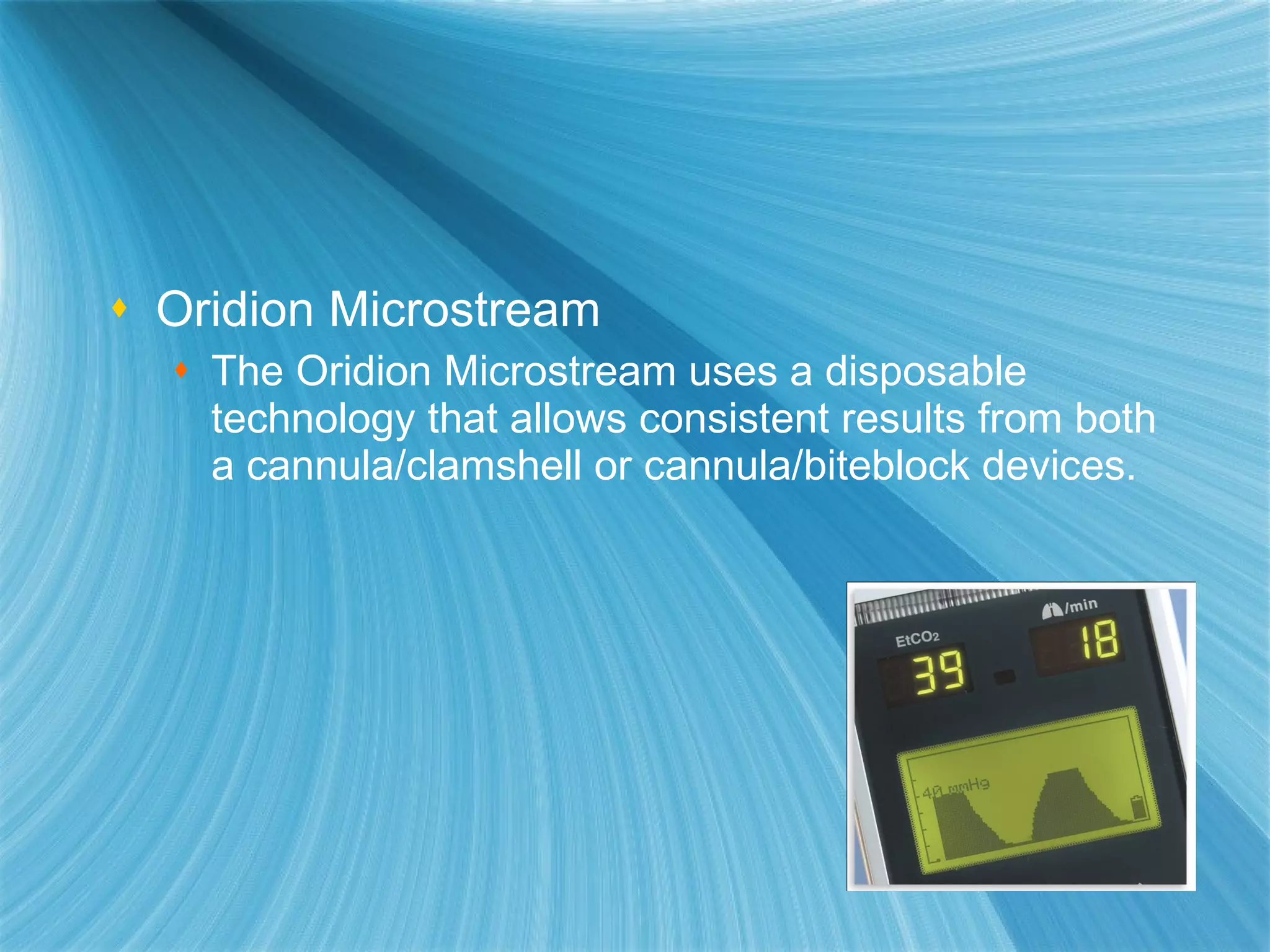
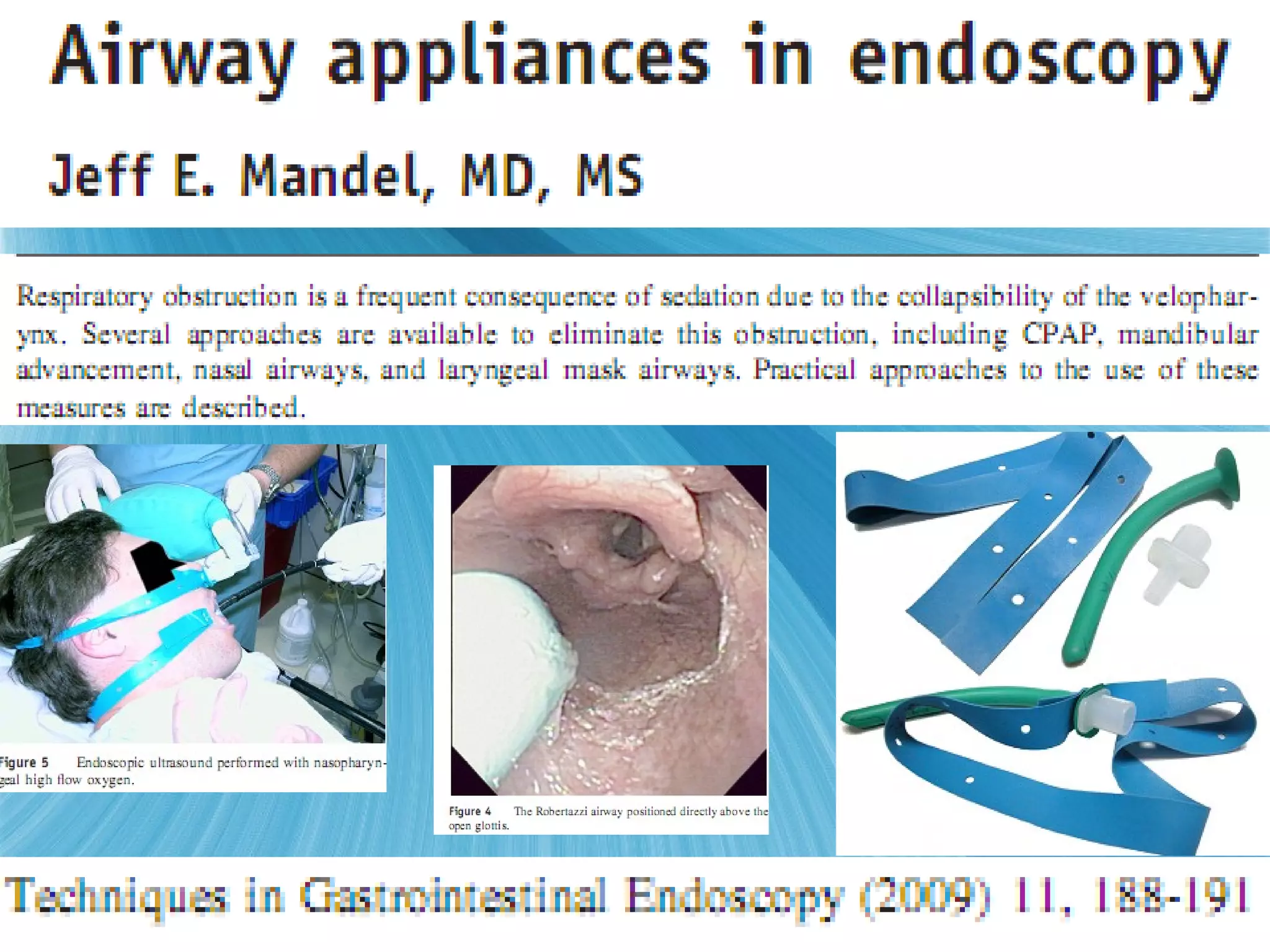
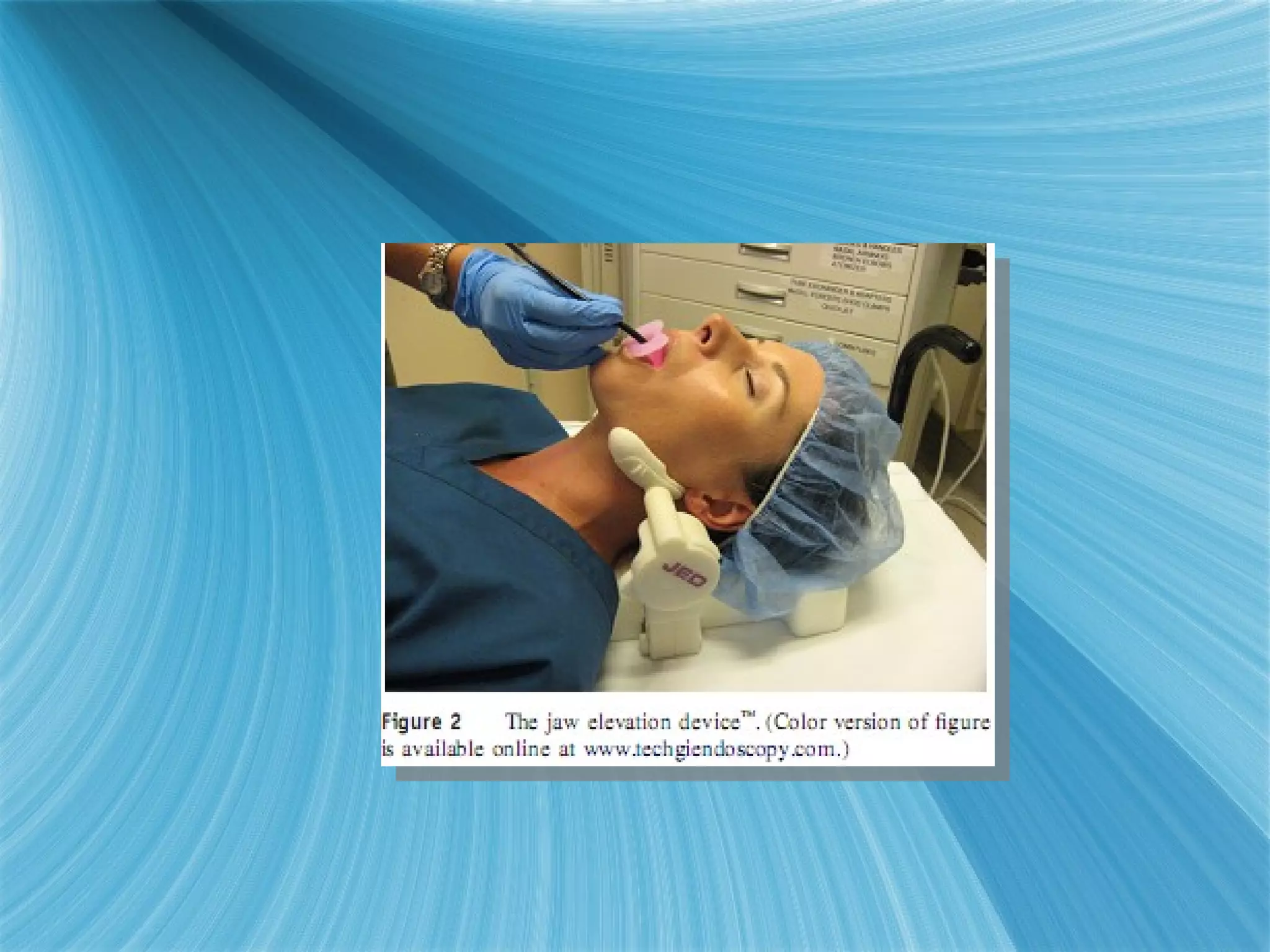
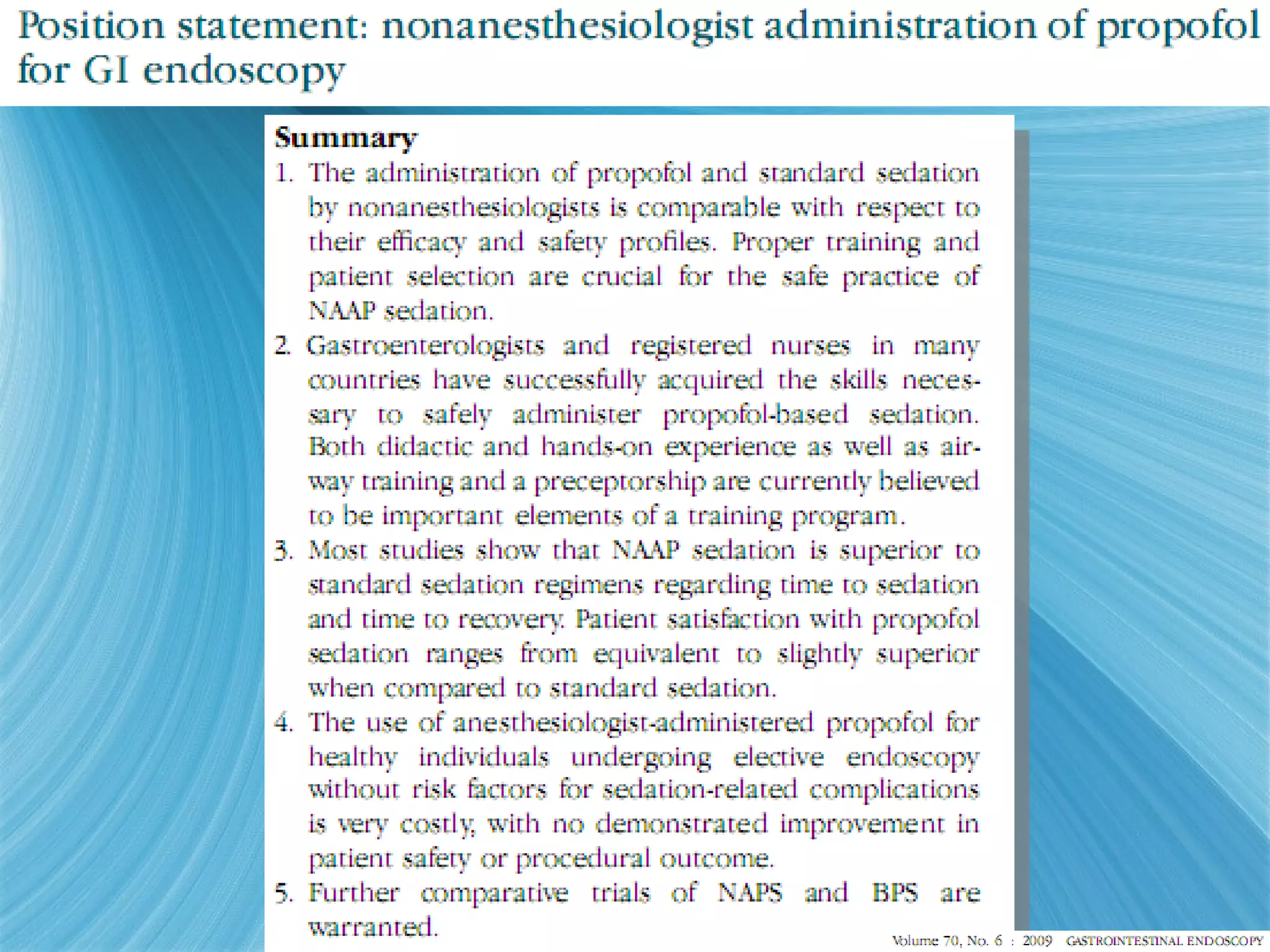
The document discusses procedural sedation and the importance of monitoring patients receiving sedation. It notes that procedural sedation aims to provide analgesia, amnesia and reduce anxiety during medical procedures. It recommends capnography as the gold standard for monitoring ventilation during sedation, as capnography can detect abnormalities in exhaled carbon dioxide levels before oxygen desaturation occurs. The document outlines various medical procedures that commonly involve procedural sedation and stresses the importance of screening patients and having proper monitoring procedures in place to protect at-risk patients during sedation.