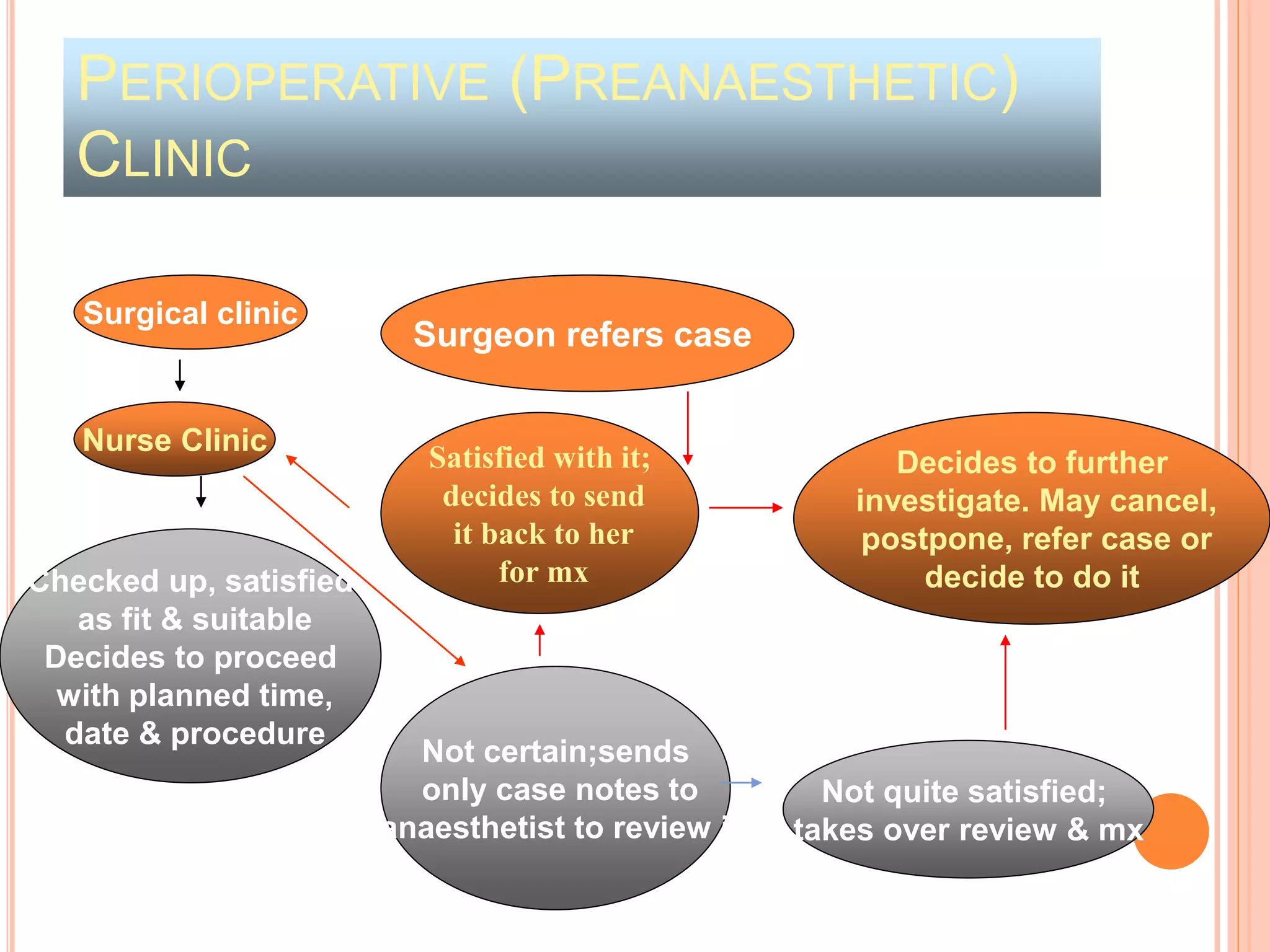
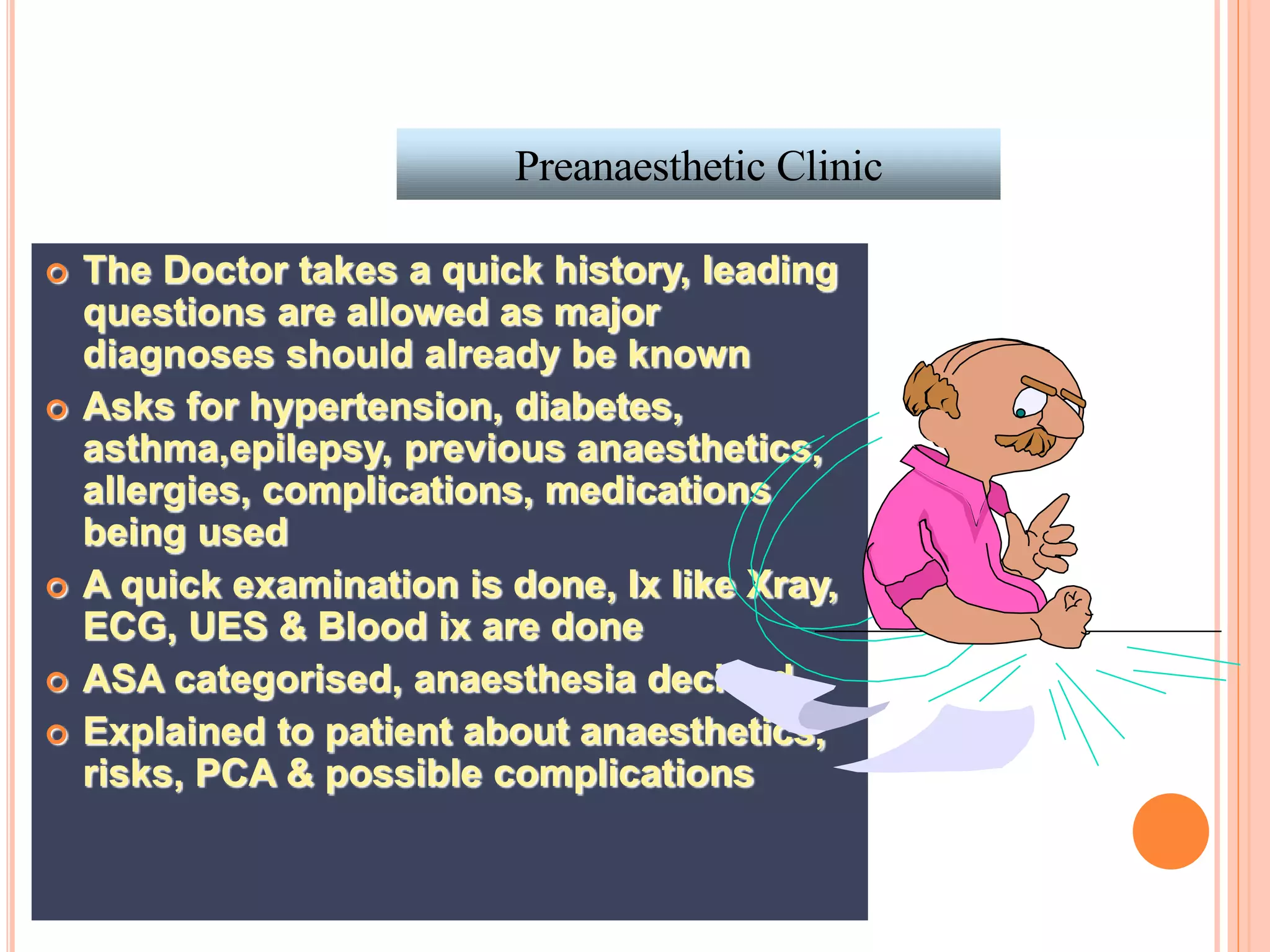
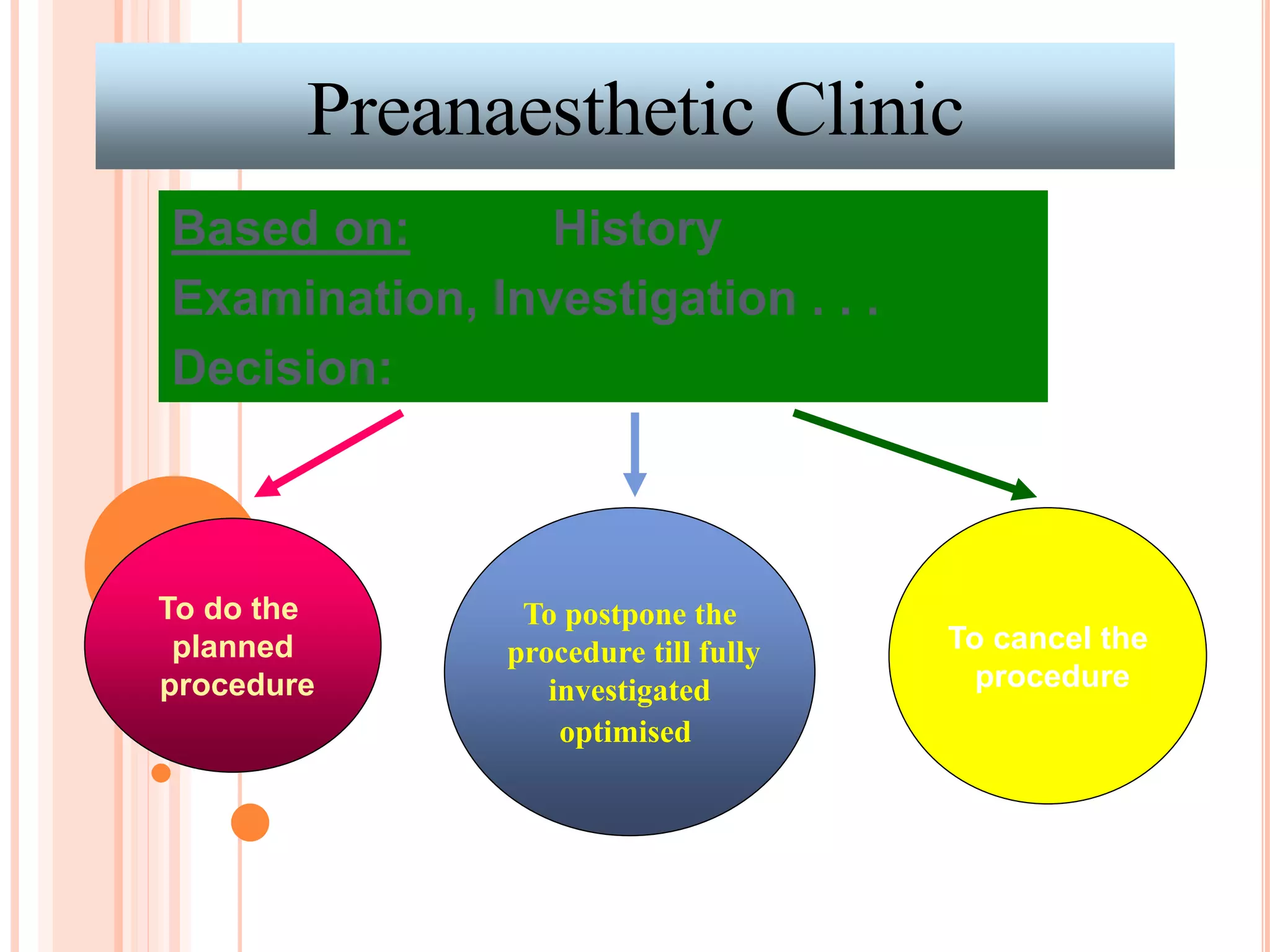
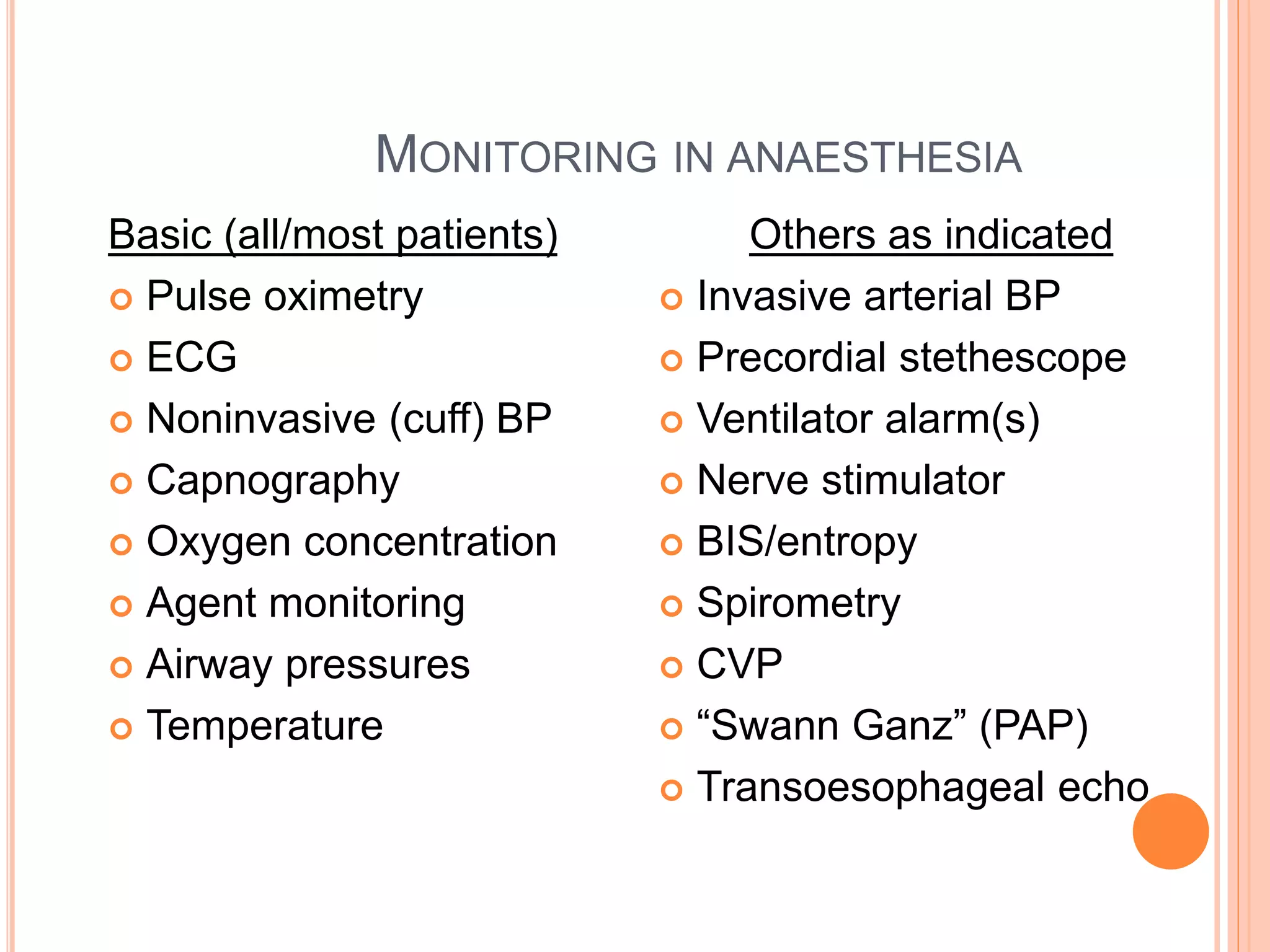
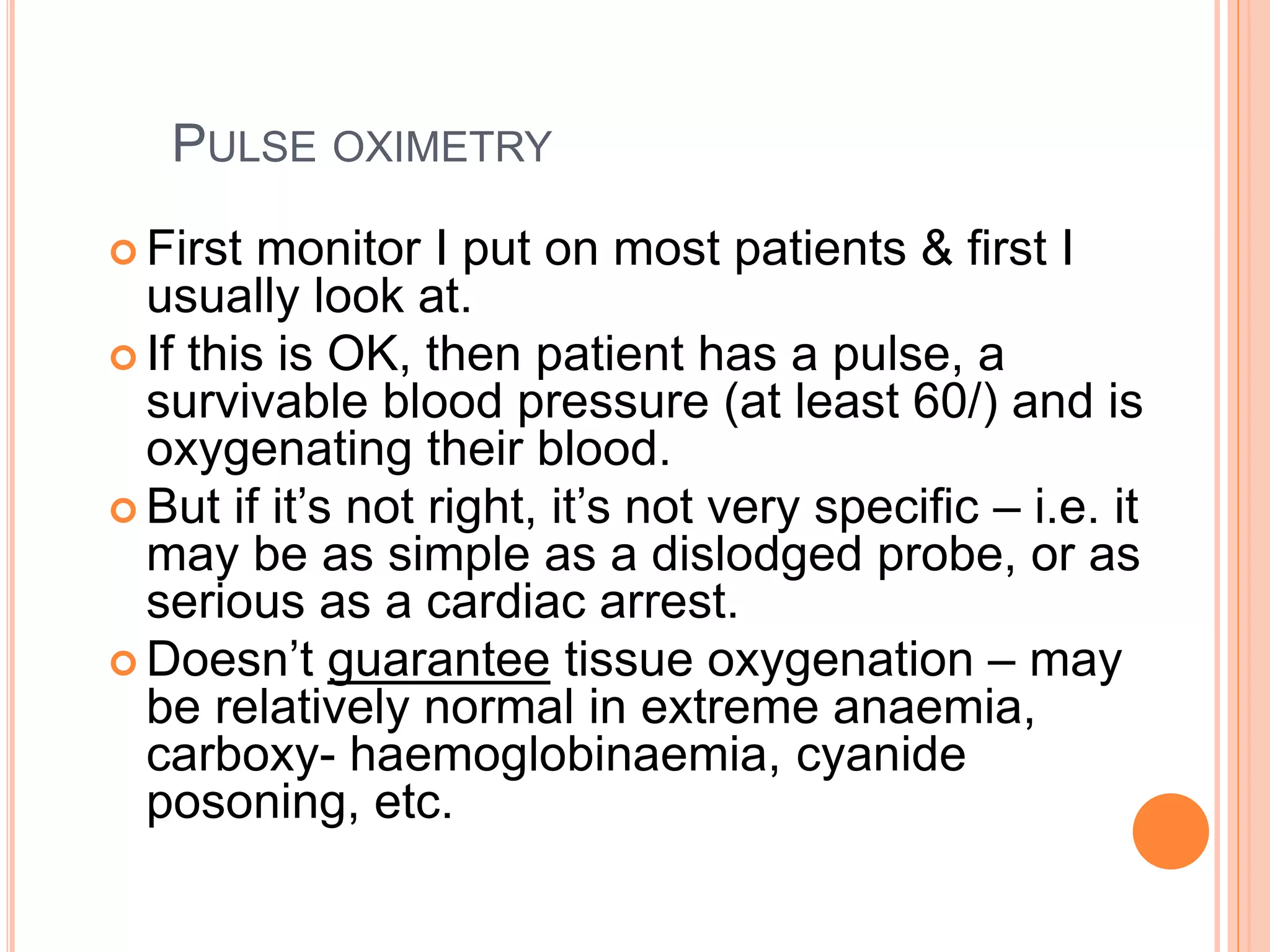
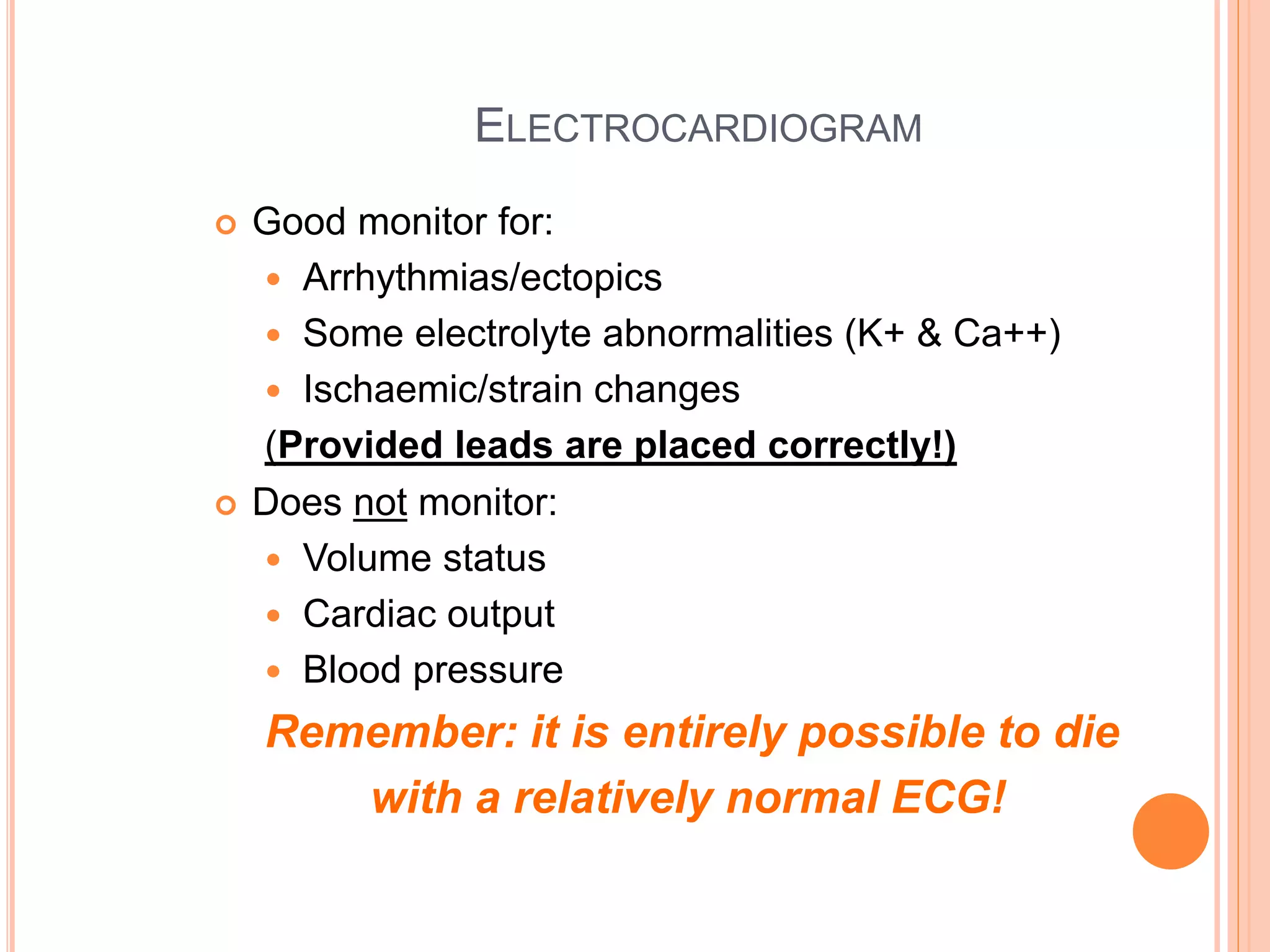
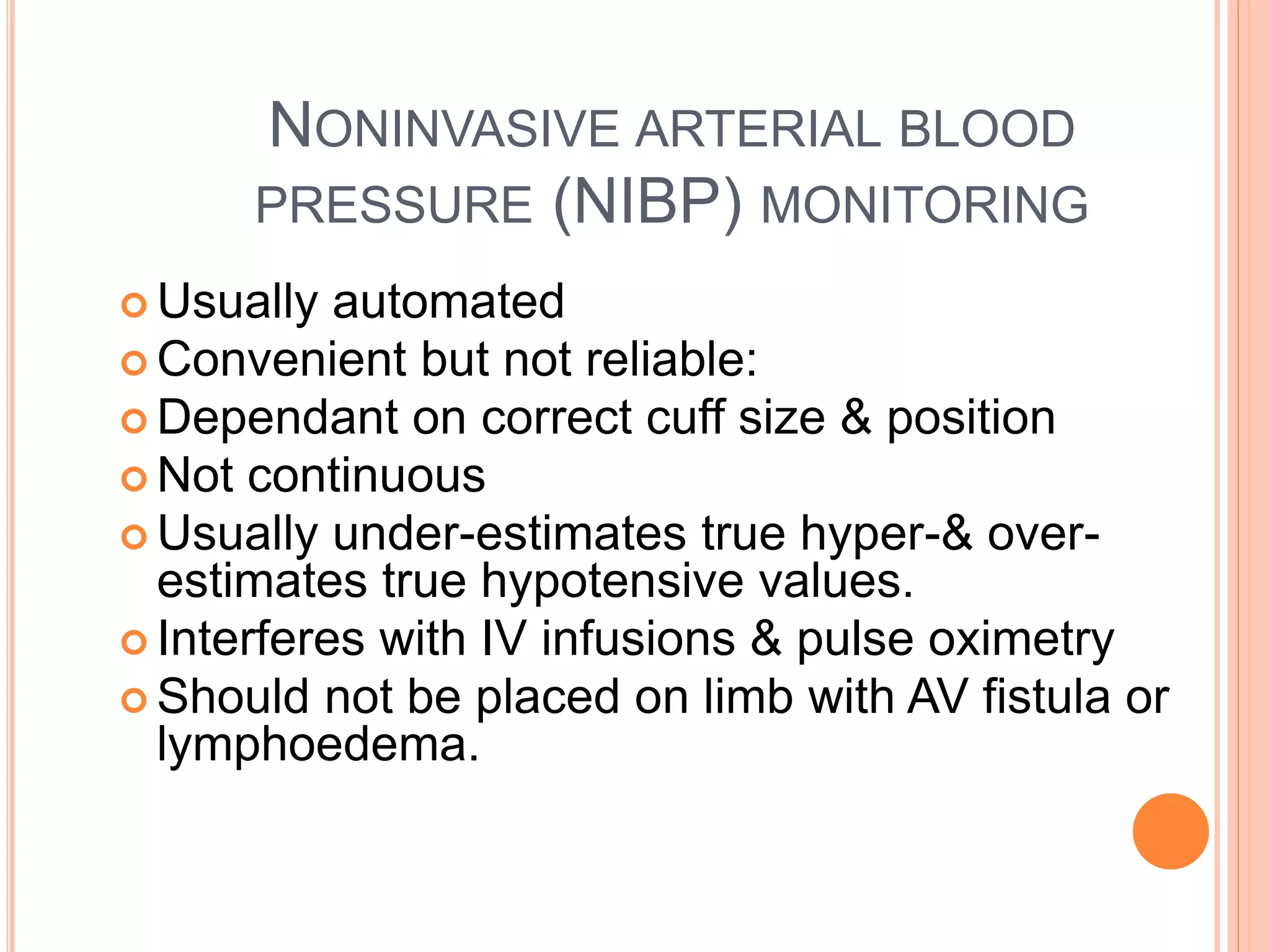
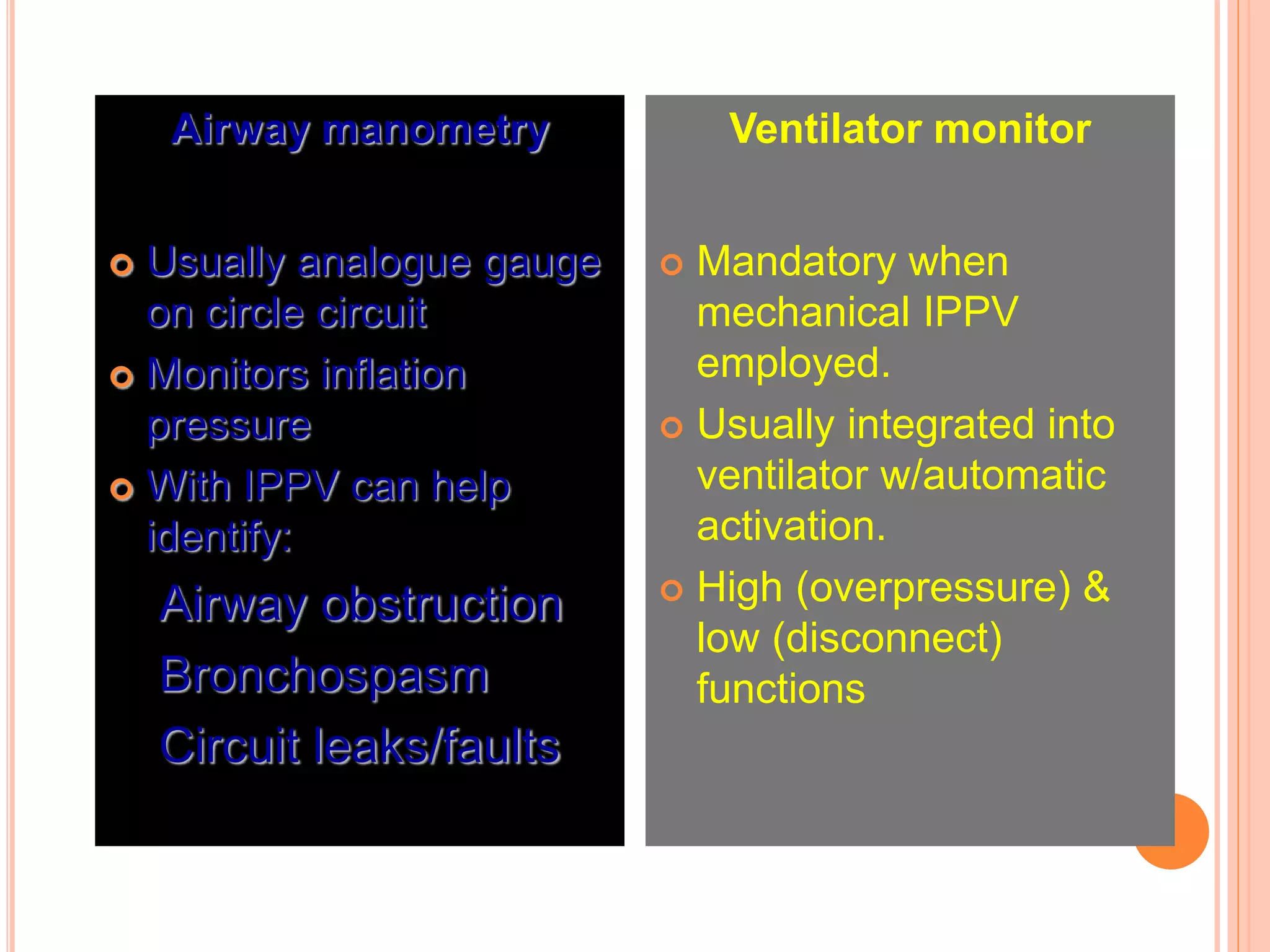
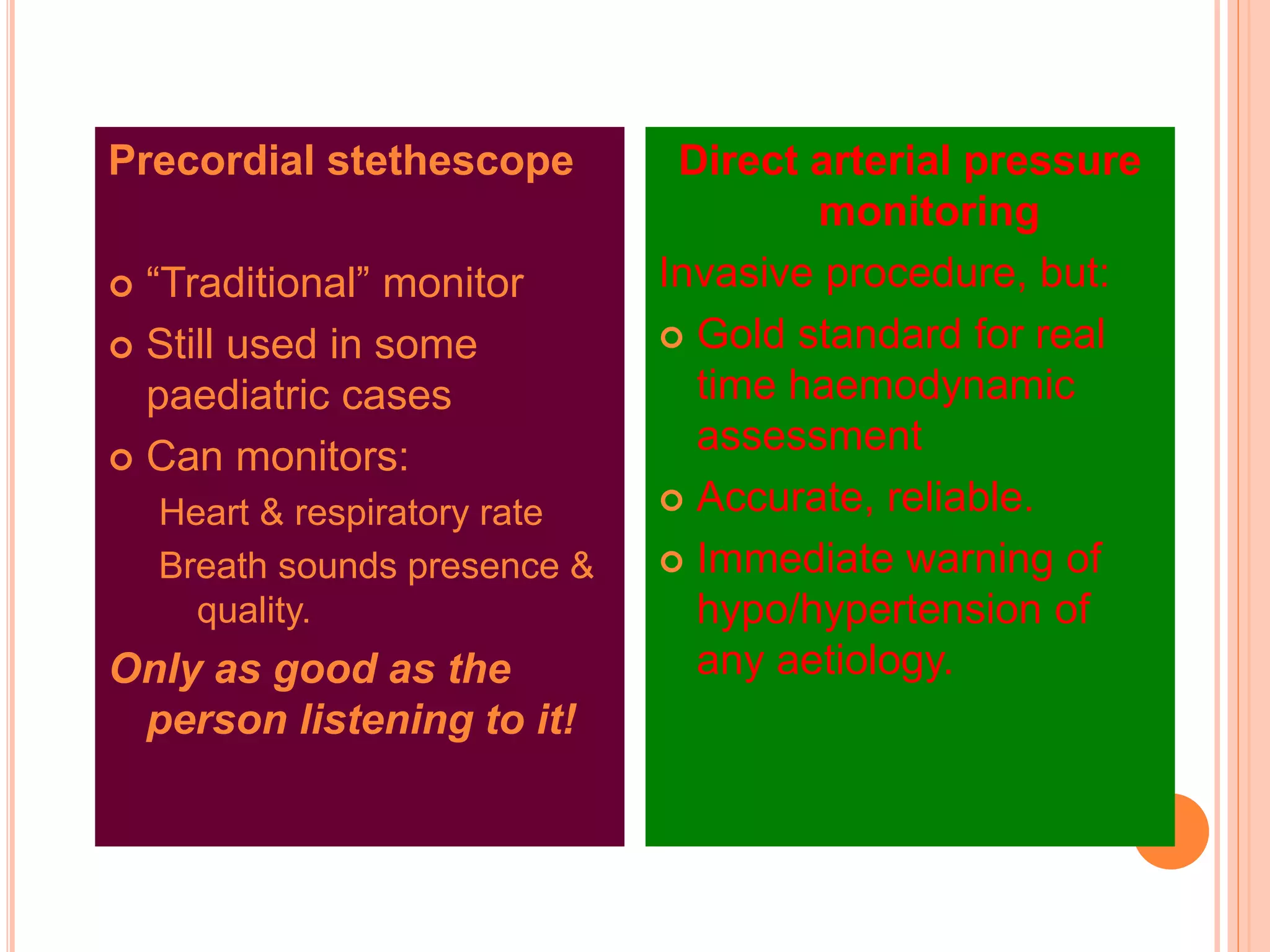
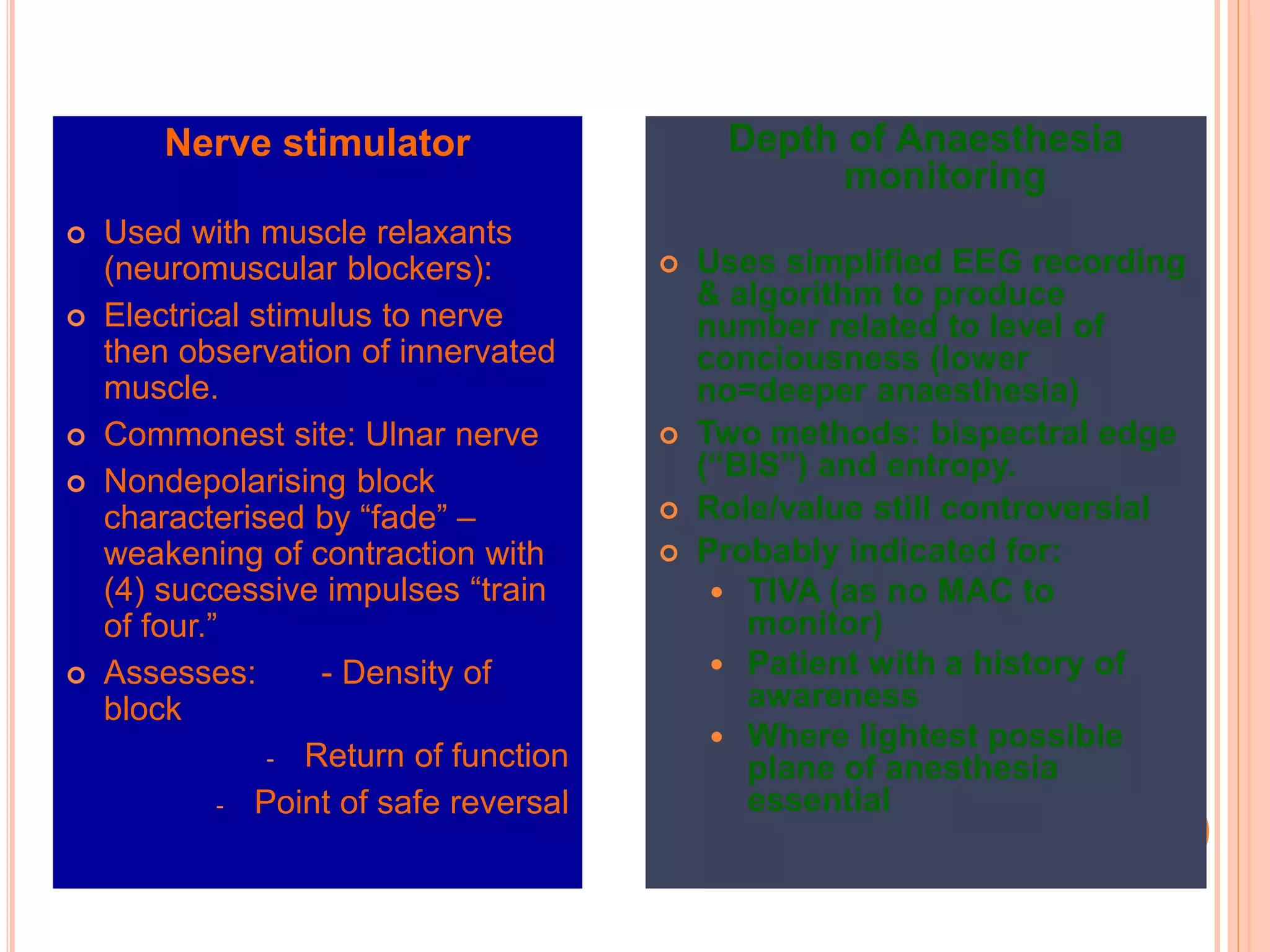
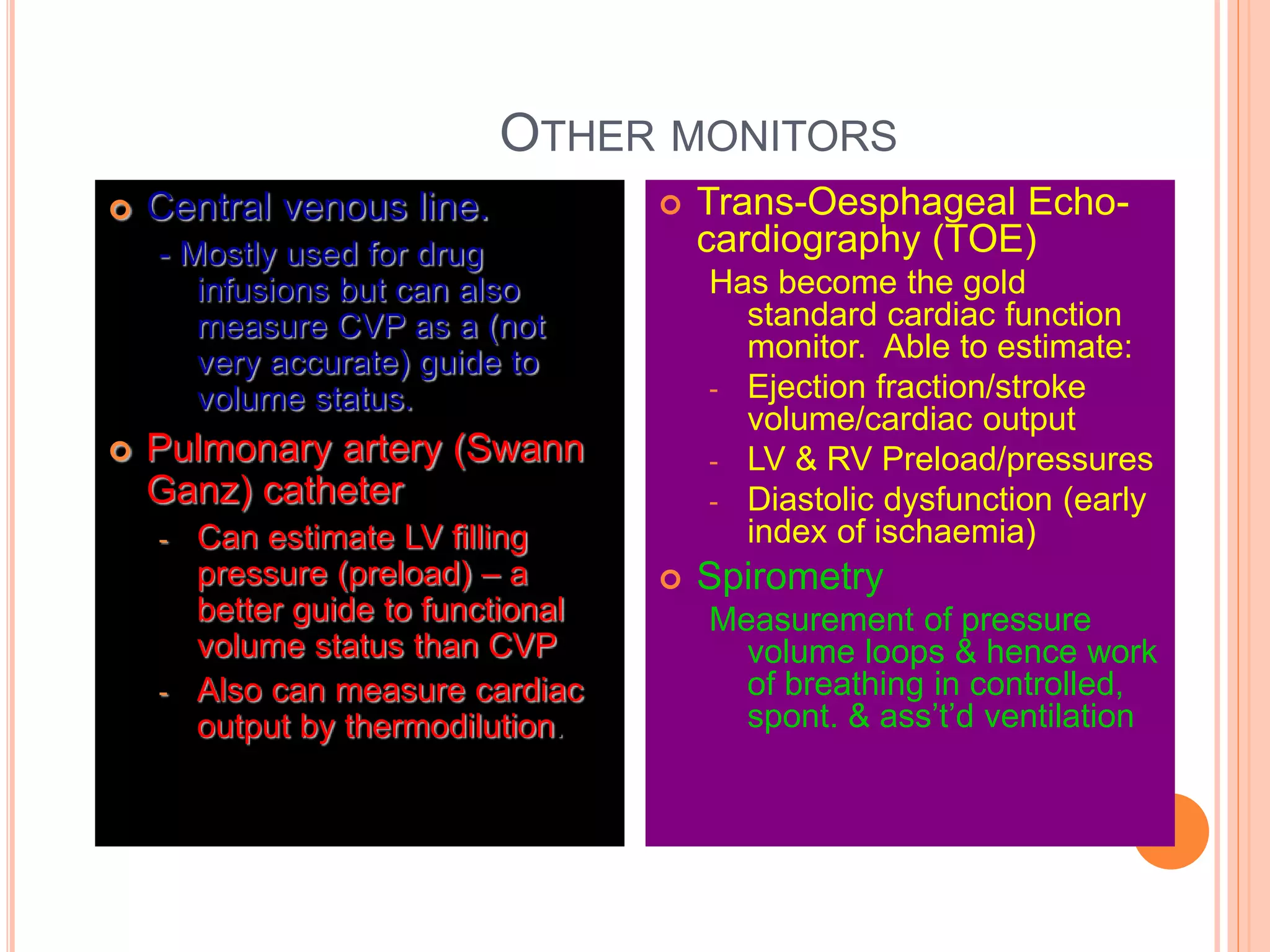
The document outlines the principles and practices of perioperative medicine, focusing on integrated multidisciplinary management of surgical patients to optimize their hospital experience and postoperative outcomes. It details the pre-anaesthetic consultation process, pre-operative preparations, and the importance of safety and monitoring during anaesthesia, including various monitoring techniques and equipment used in practice. Additionally, it emphasizes the significance of risk assessment and patient optimization before surgery to ensure safety and effective management in anaesthesia.