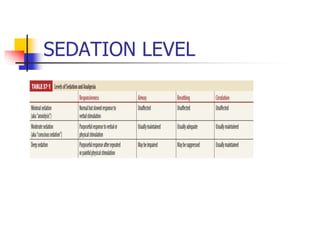
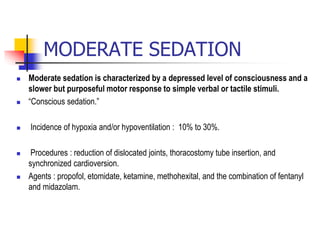
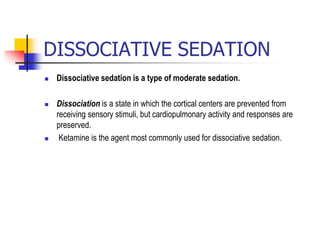
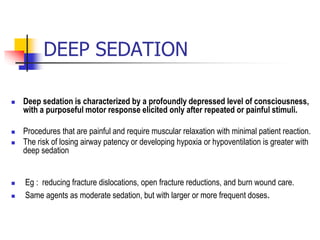
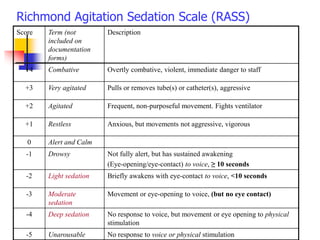
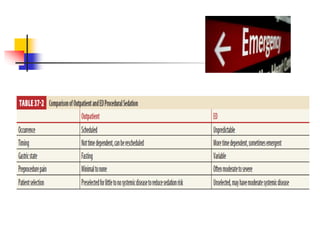
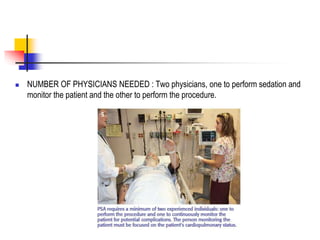
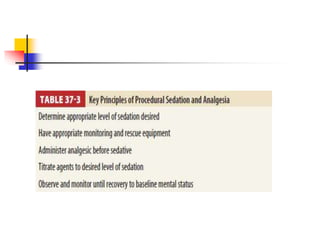
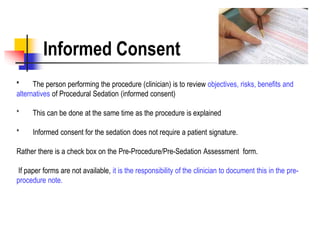
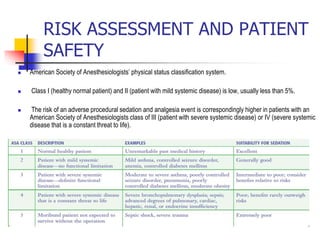
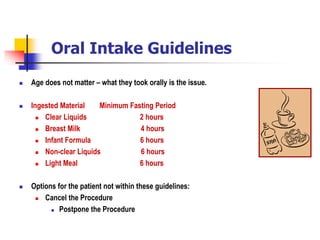
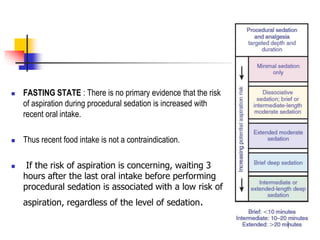
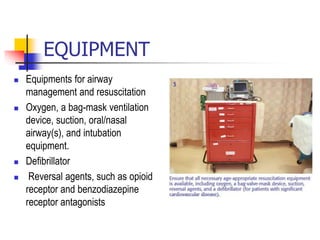
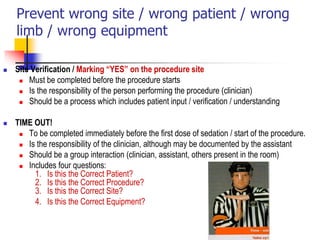
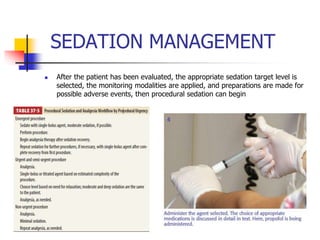
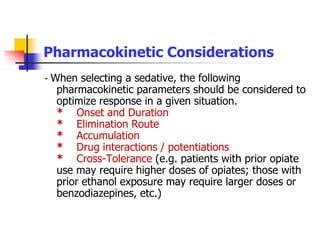
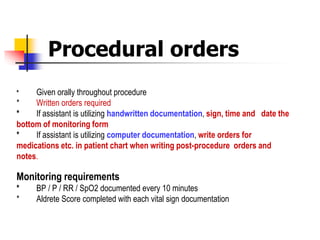
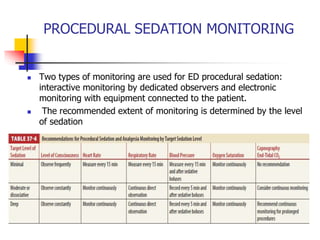
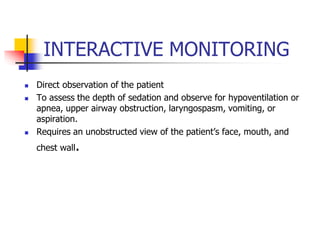
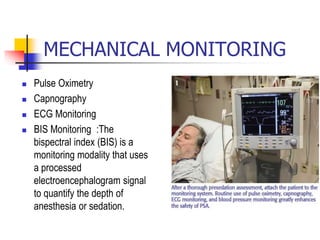
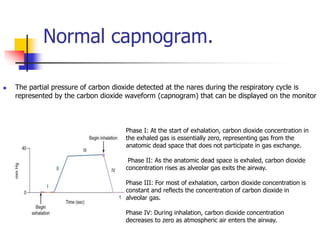
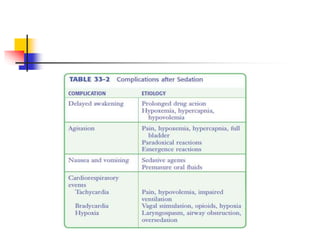
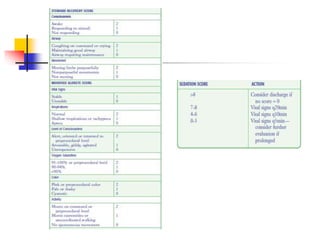
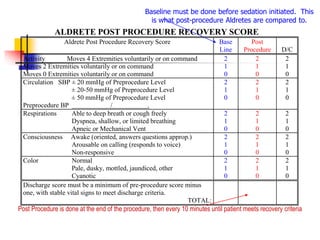
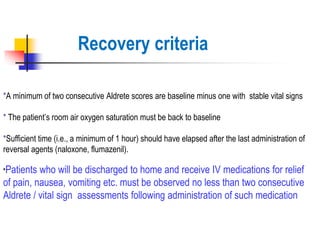
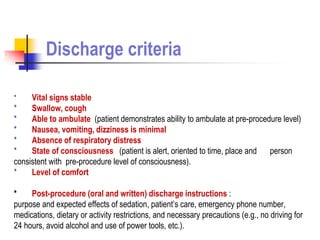
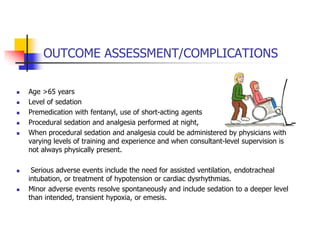
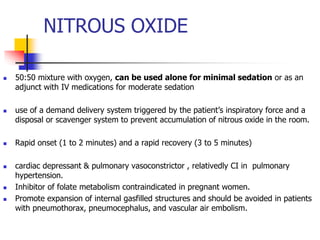
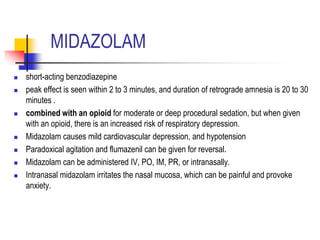
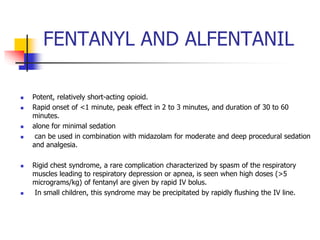
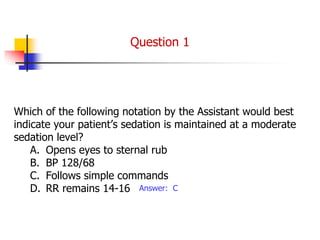
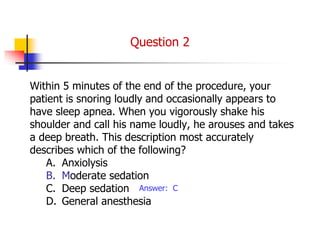
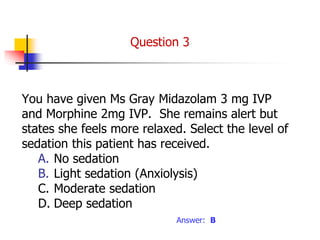
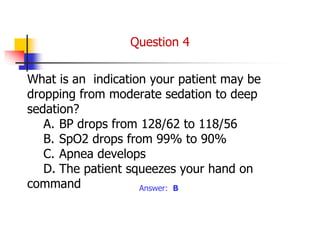
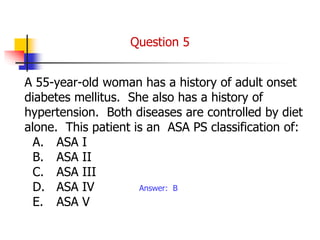
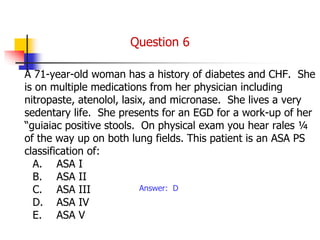
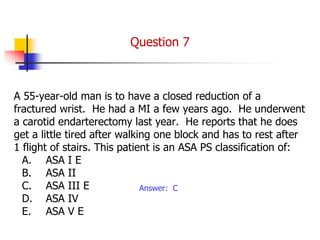
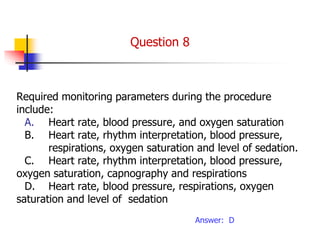
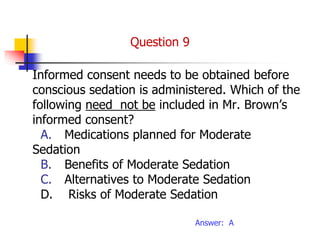
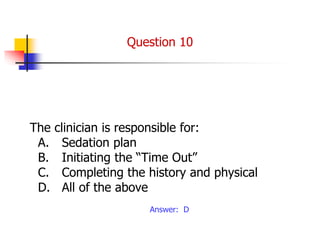
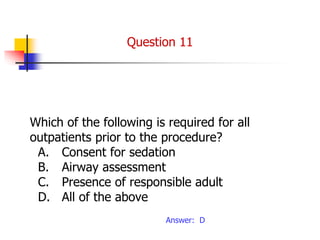
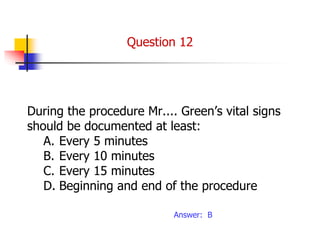
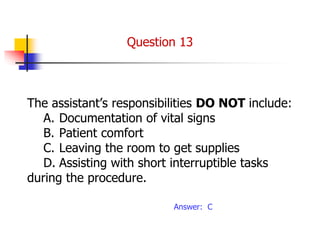
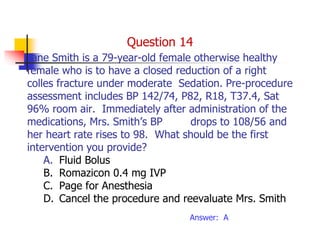
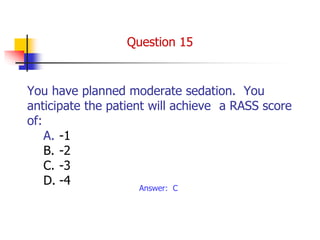
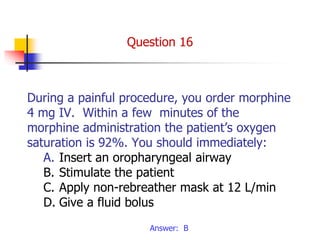
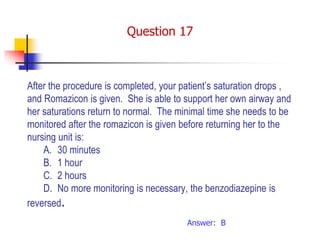
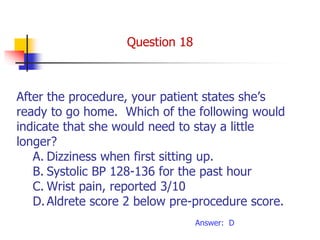
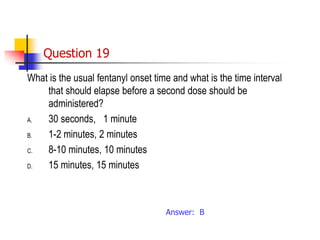
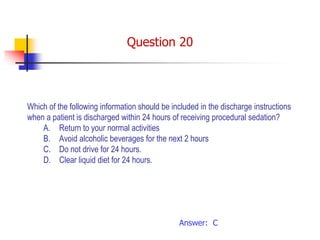
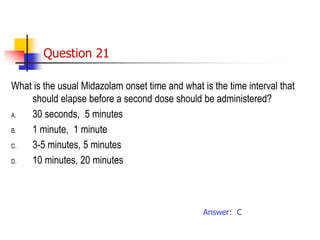
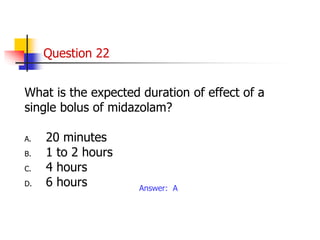
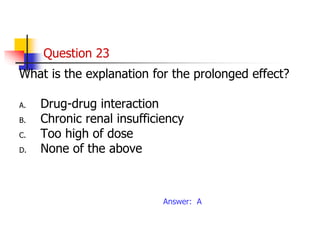
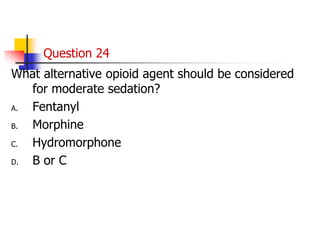
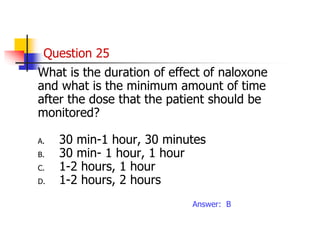
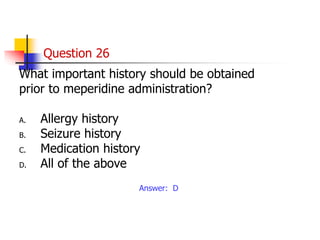
The document discusses procedural sedation, including definitions of different levels of sedation, monitoring requirements, safety considerations, common sedating agents like nitrous oxide, midazolam, fentanyl and their properties, and discharge criteria after a procedure. Procedural sedation involves administering sedatives to induce a depressed level of consciousness while maintaining cardiorespiratory function to allow medical procedures with little patient reaction or memory.