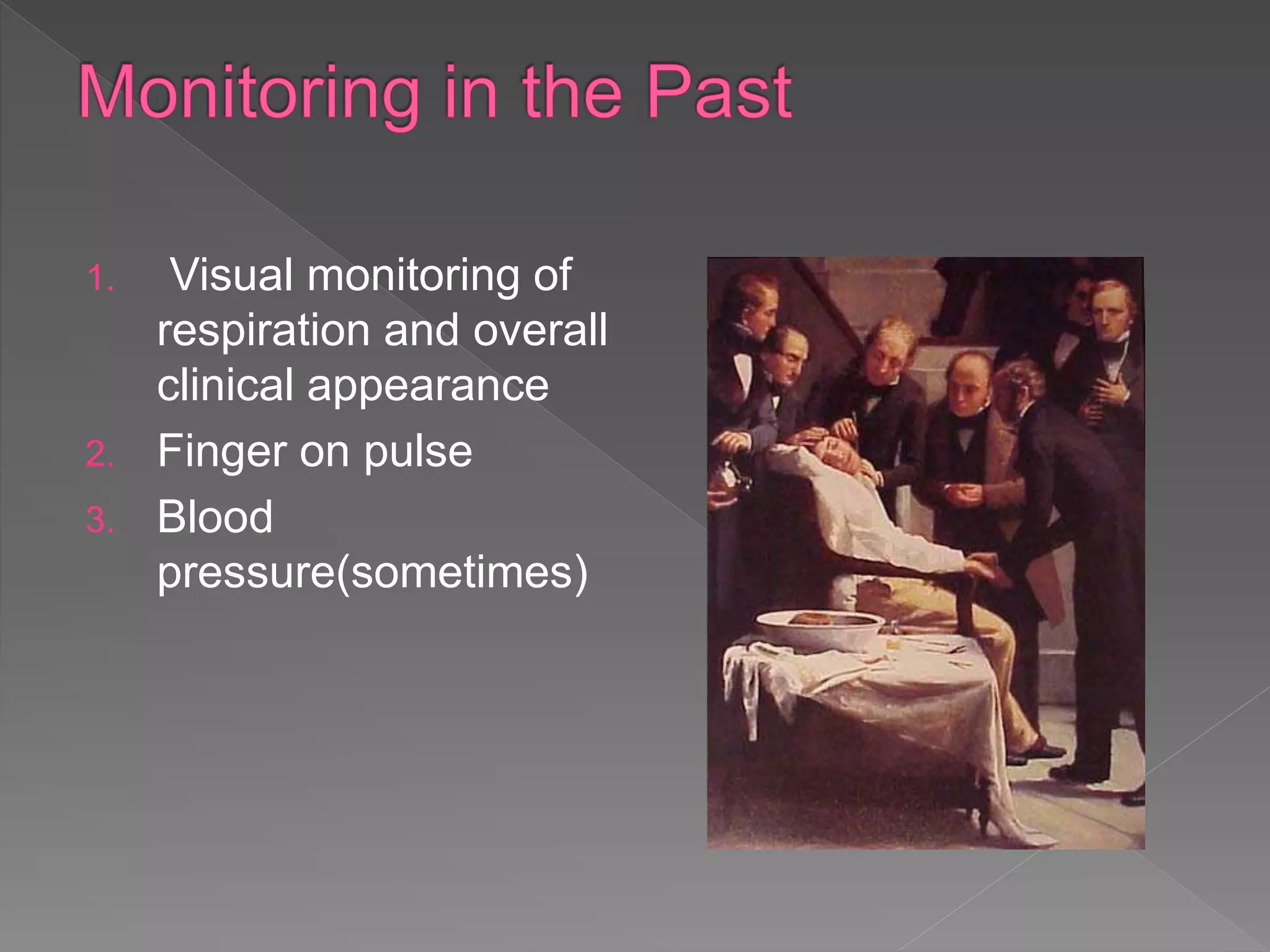
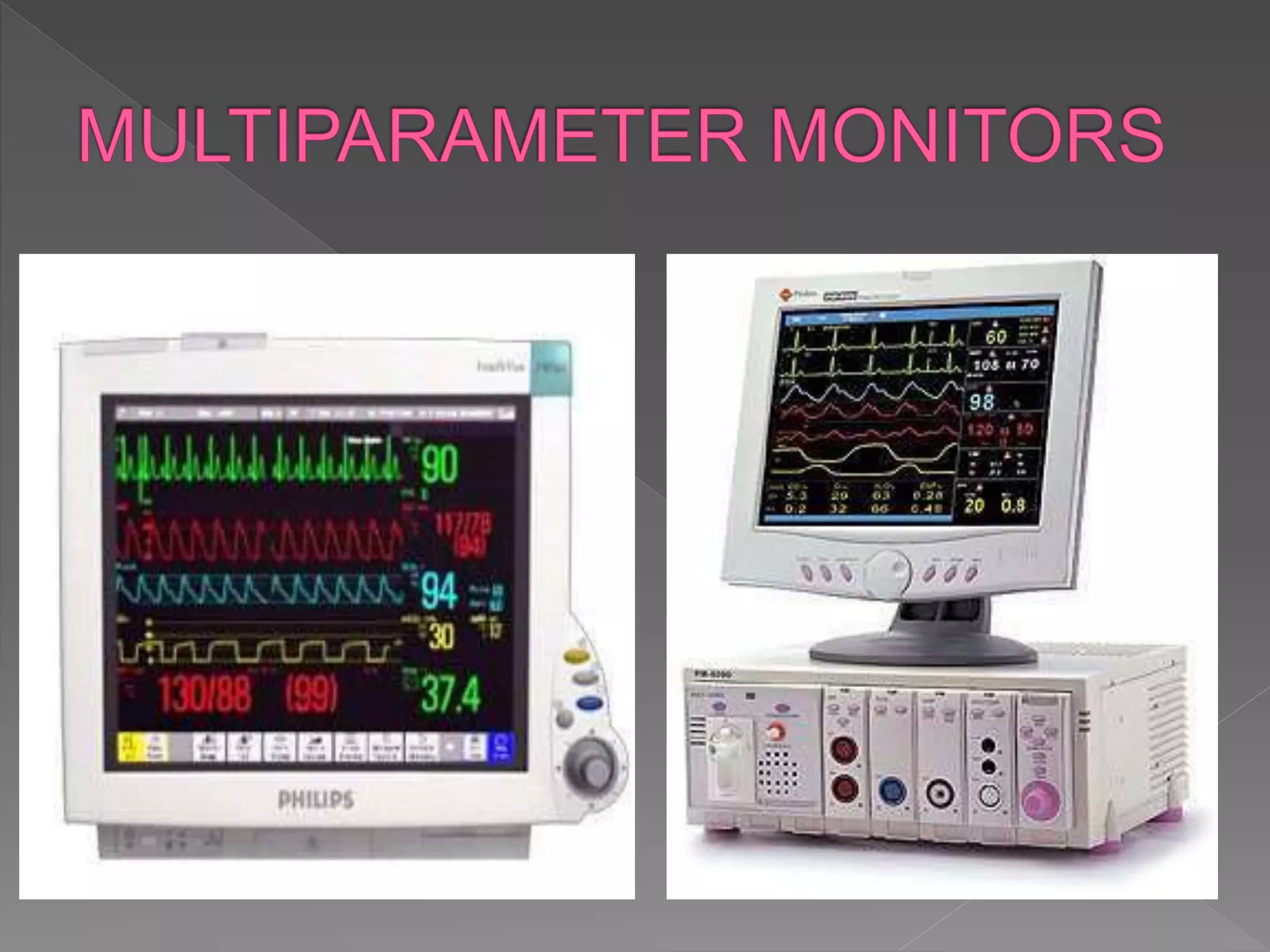
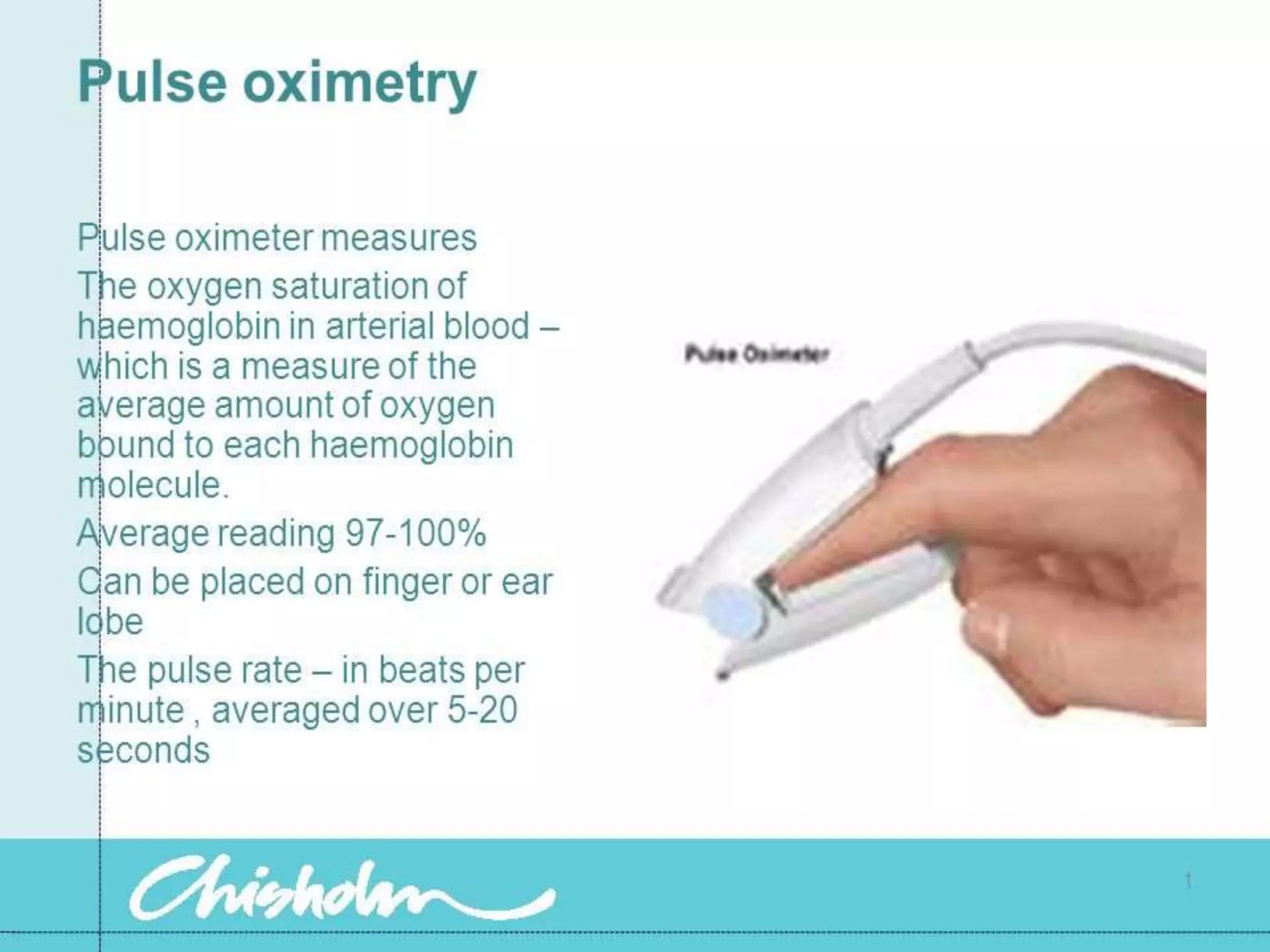
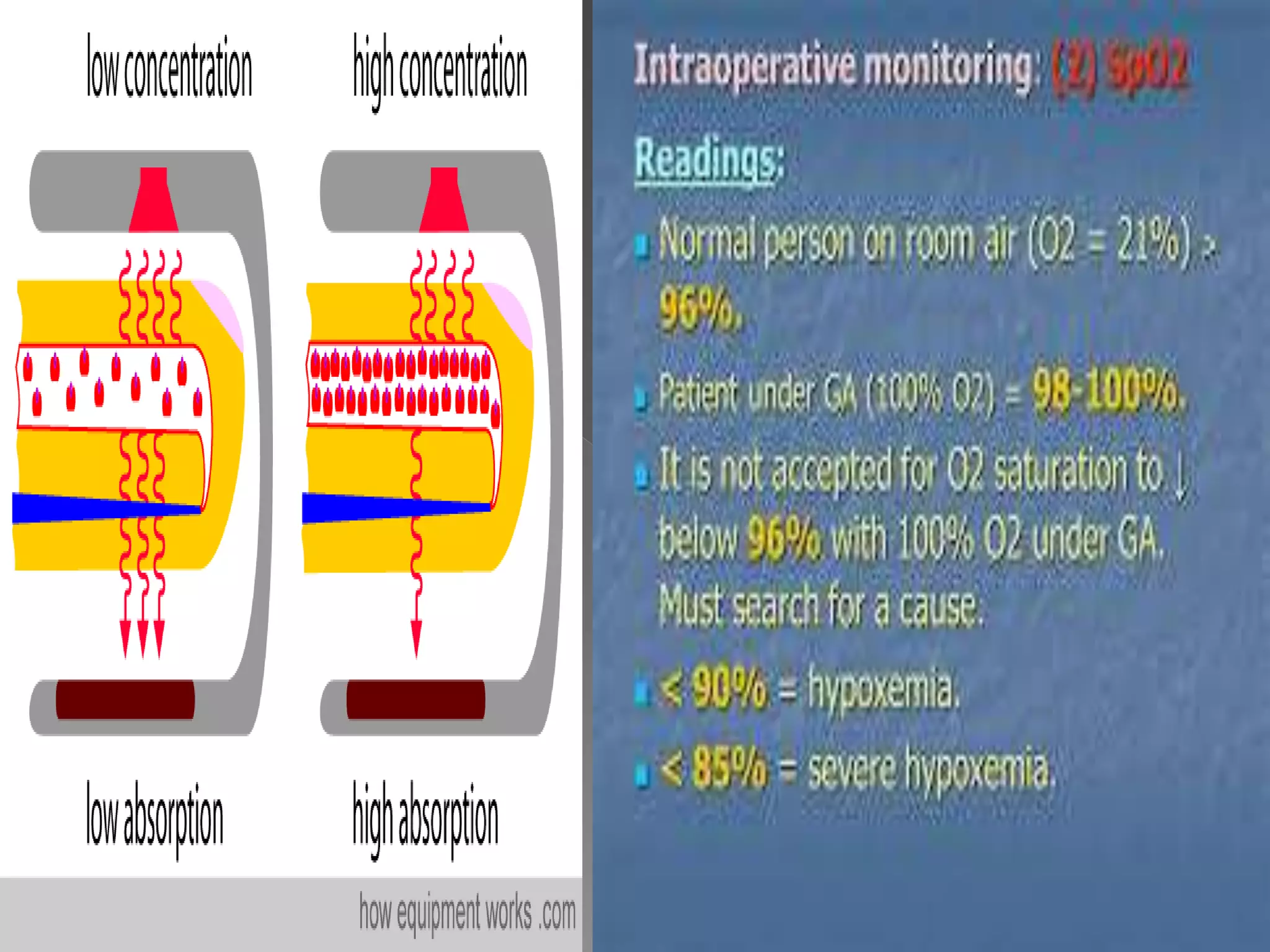
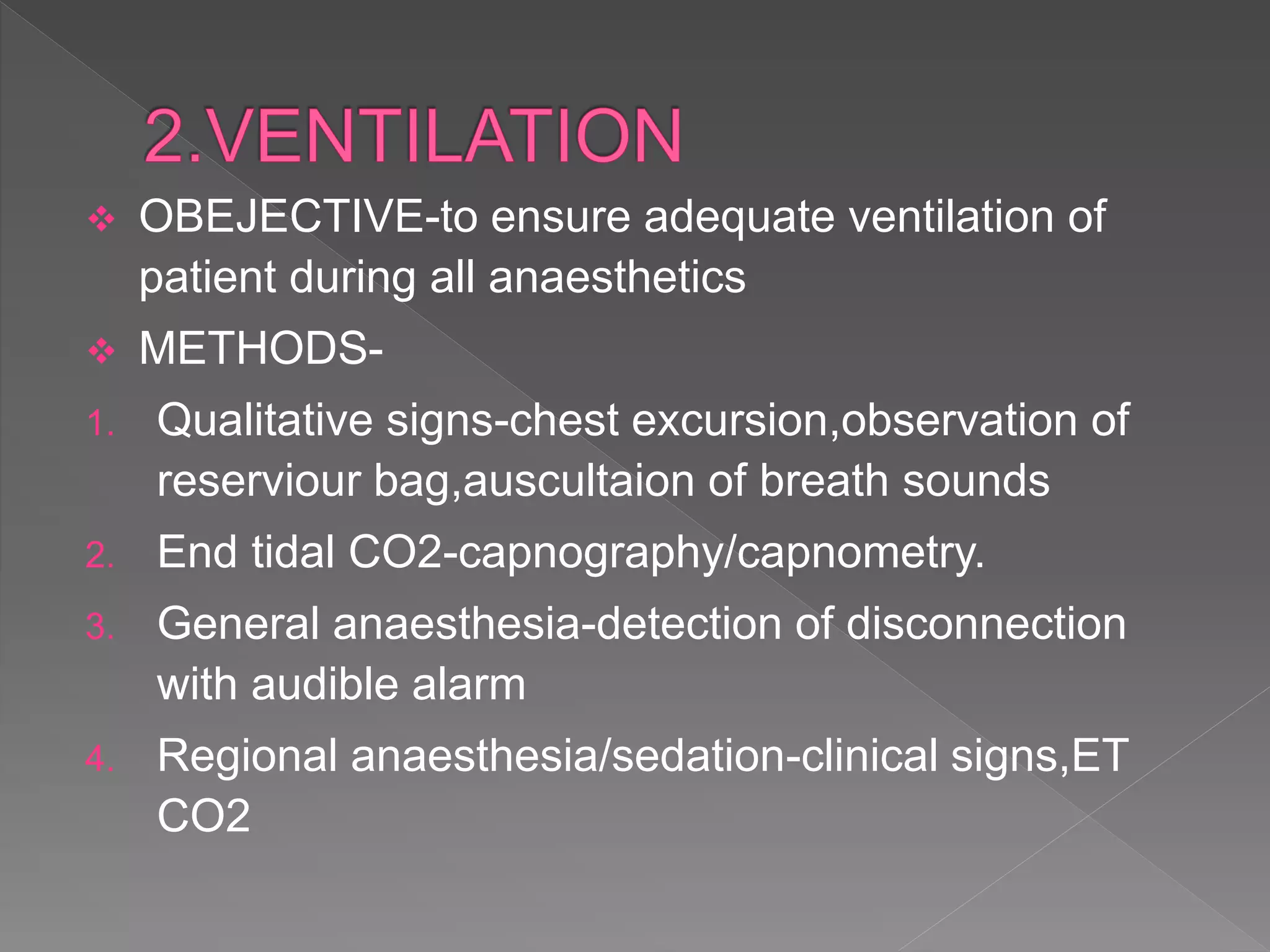
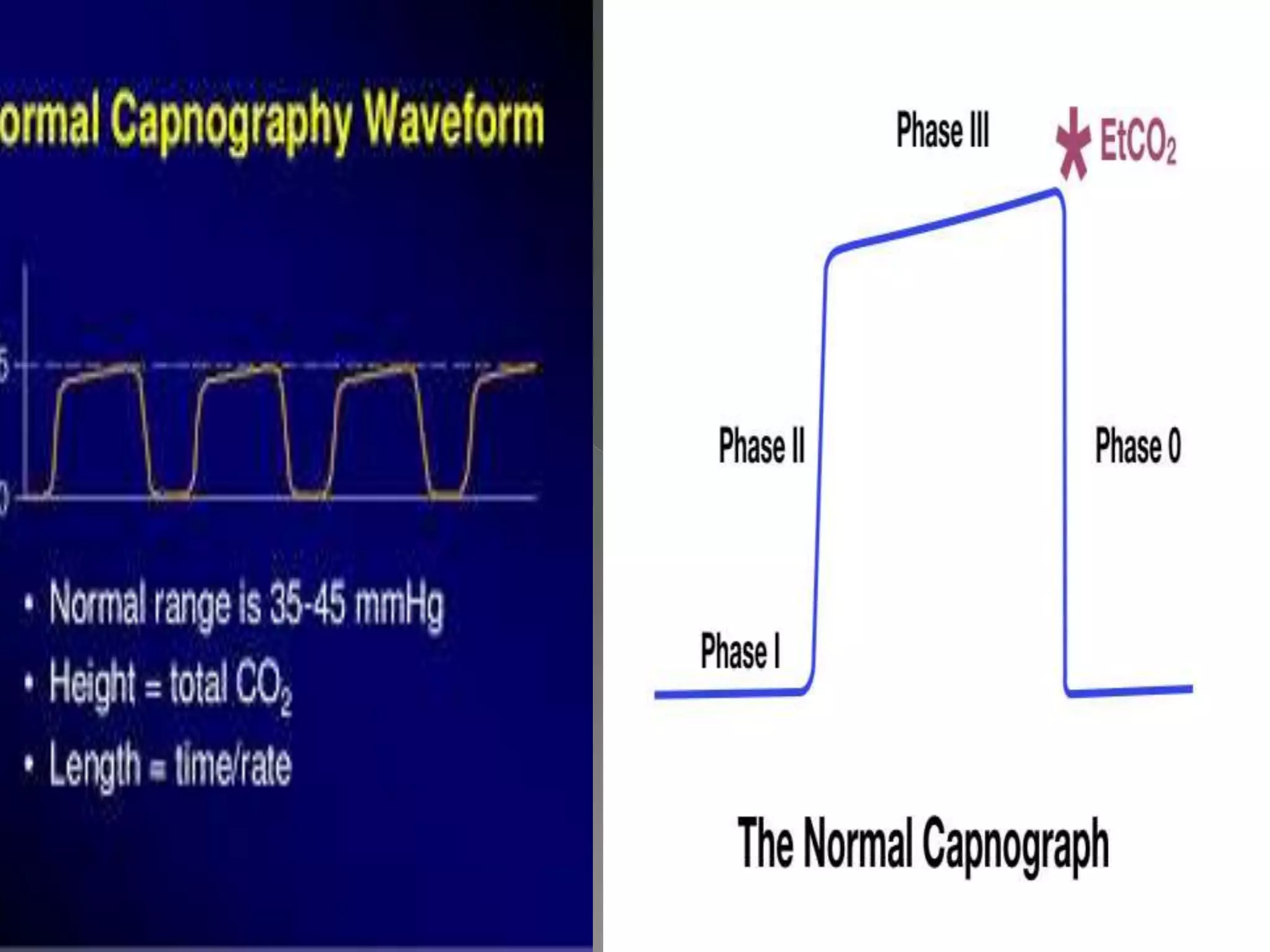
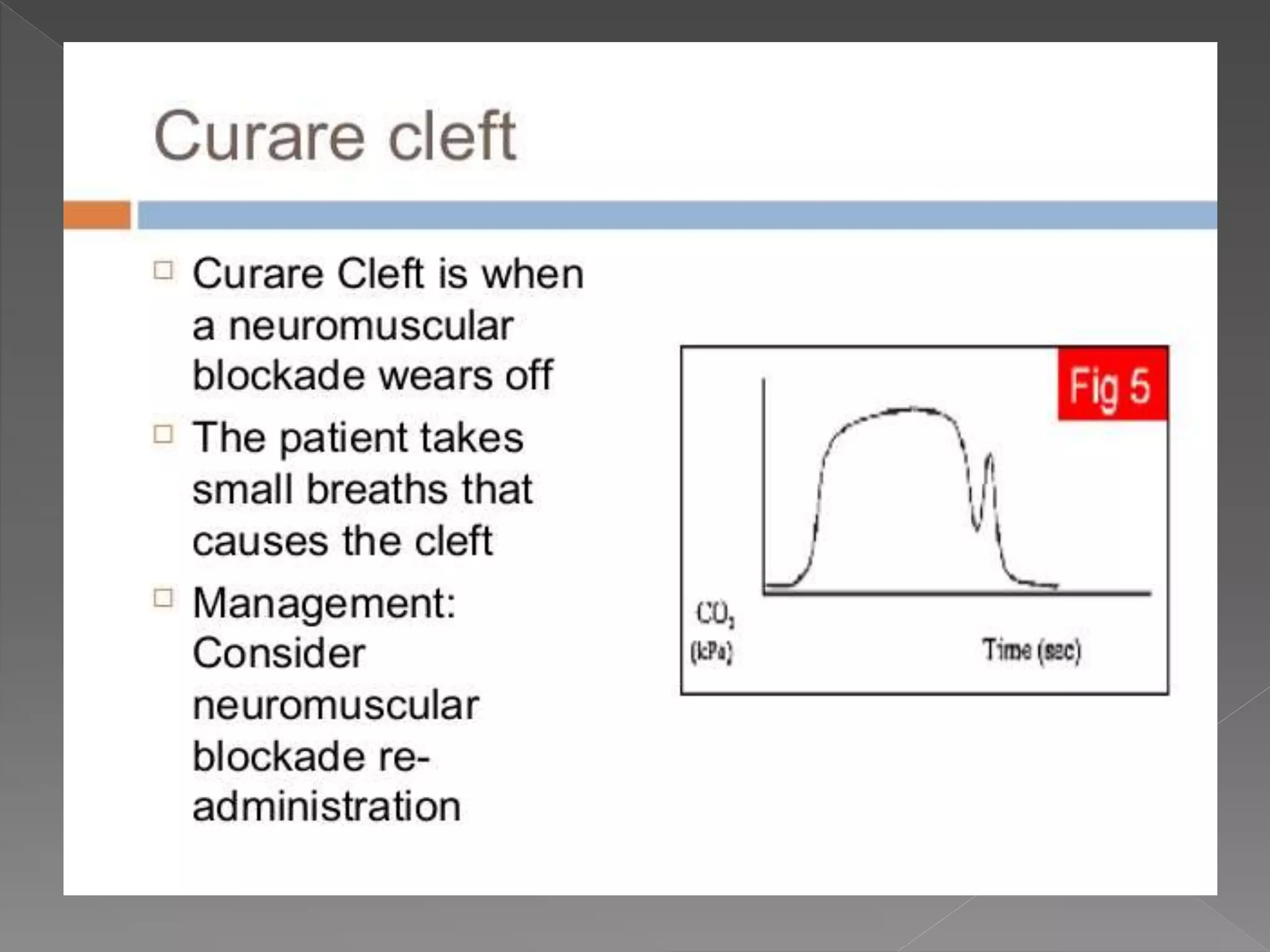
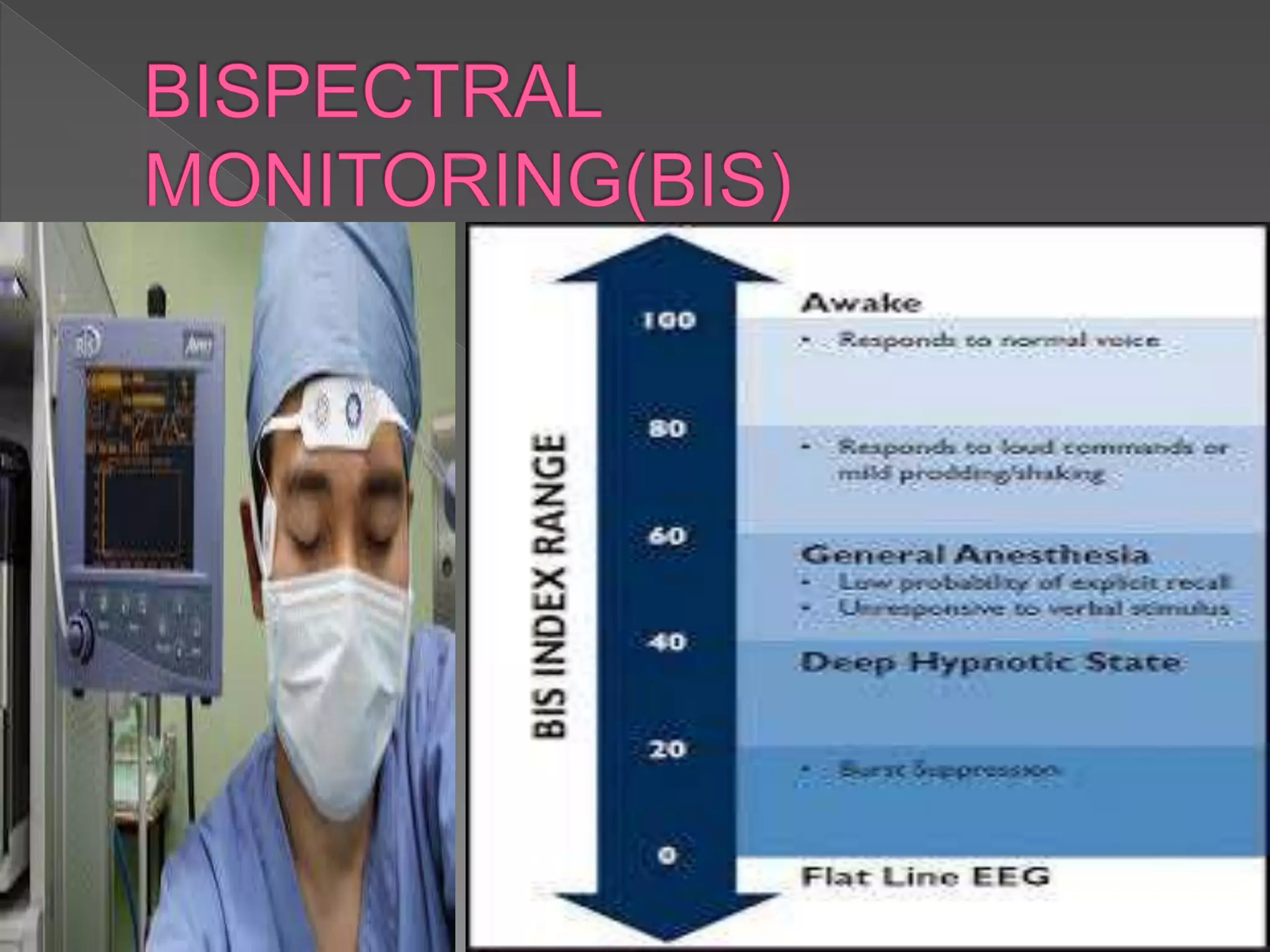
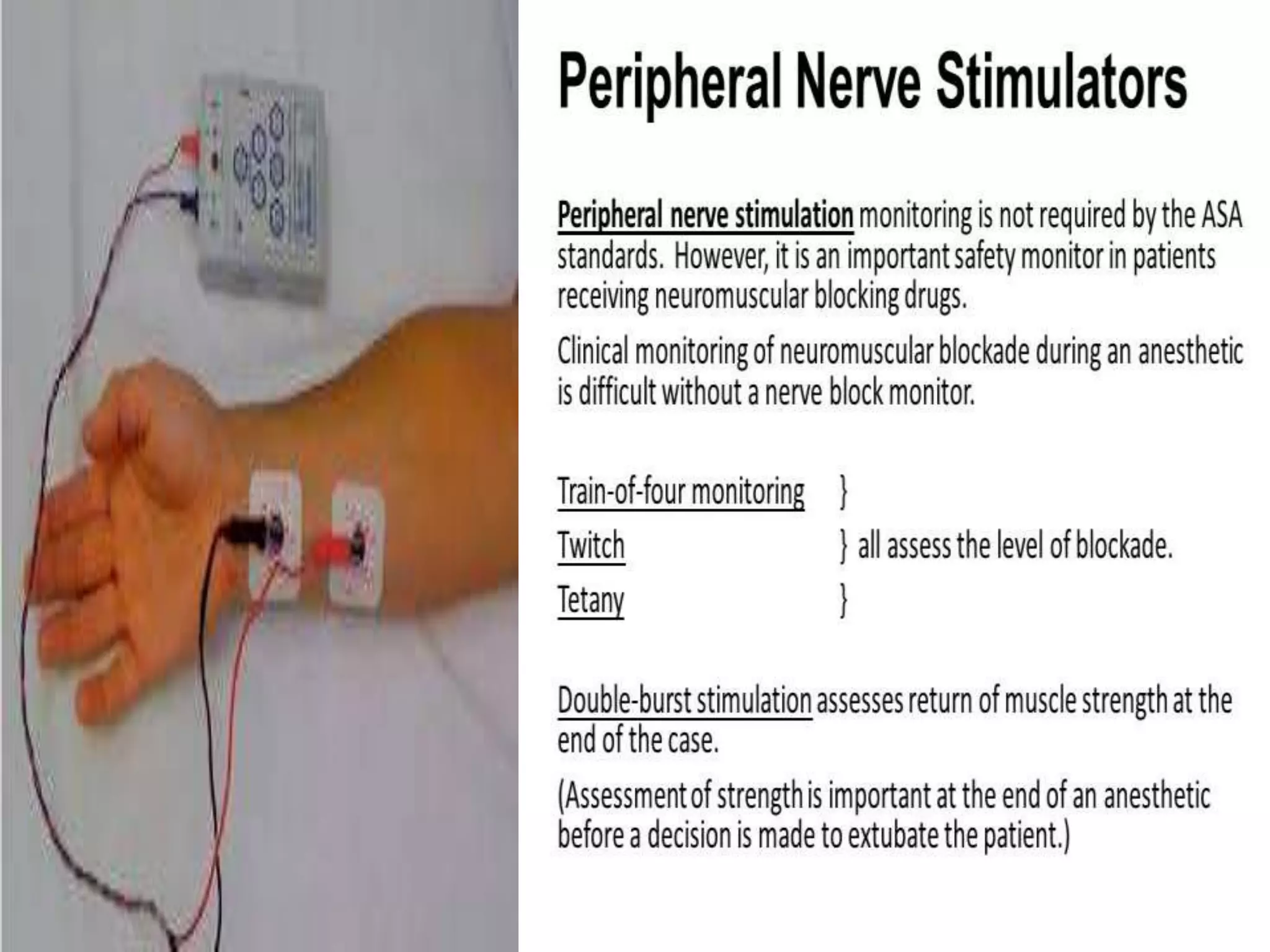
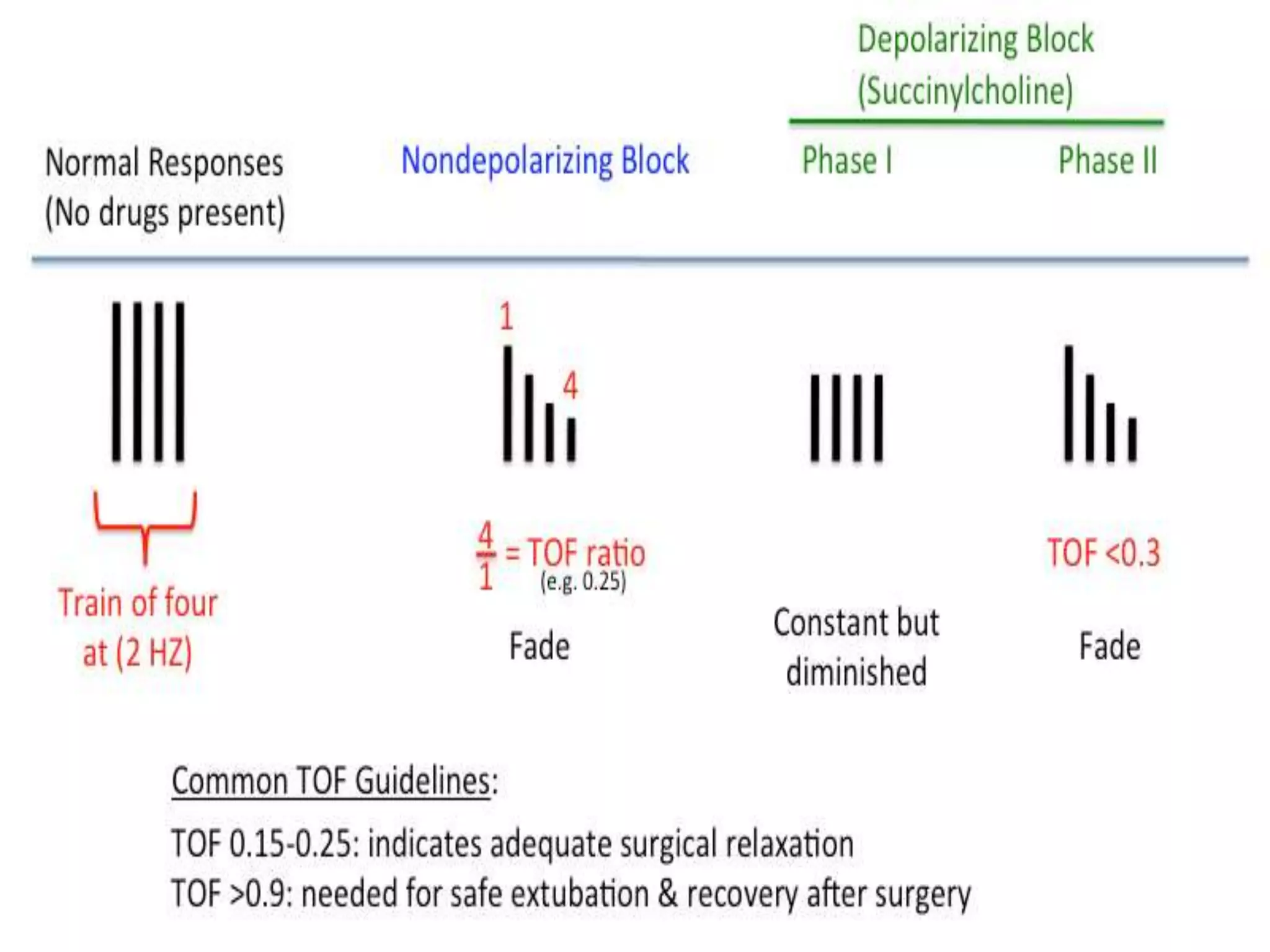
This document discusses the importance of monitoring patients during anesthesia. It states that the primary goal of monitoring is to keep patients as safe as possible during surgery by evaluating their oxygenation, ventilation, circulation, and temperature throughout the procedure. Proper monitoring can reduce risks such as hypoventilation, equipment malfunctions, and physiological imbalances. The document outlines the American Society of Anesthesiologists' guidelines for standard monitoring, including continuous evaluation of respiration, pulse oximetry, end-tidal carbon dioxide, electrocardiography, blood pressure, temperature, depth of anesthesia, muscle relaxation, and urine output. It emphasizes that while machines are helpful aids, the most important monitor is the presence of qualified anesthesia personnel.