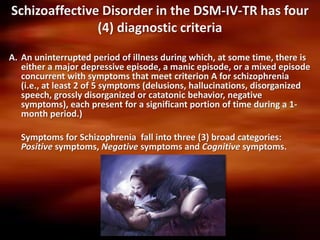
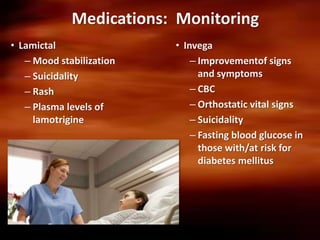
This case presentation discusses a 50-year-old African American female patient admitted to the hospital for schizoaffective disorder, manic episode. The patient has a history of schizoaffective disorder and has been living in a nursing home. The goals of hospitalization are to decrease restlessness, irritability, worry, anxiety and increase self-control and medication compliance. Interventions include medication management with Lamictal and Invega, nursing care, social work support, and education. The presentation provides context on schizoaffective disorder, symptoms, course, and treatment goals for managing the manic episode.