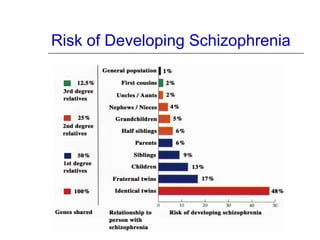
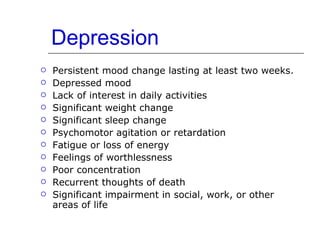
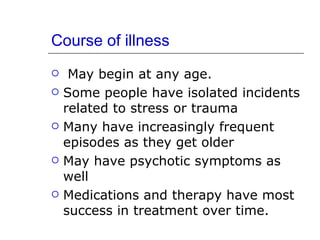
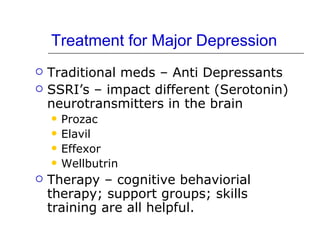
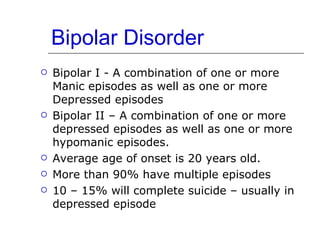
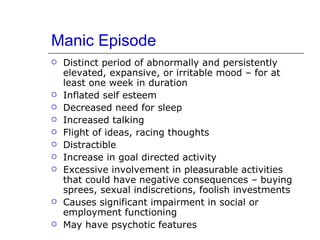
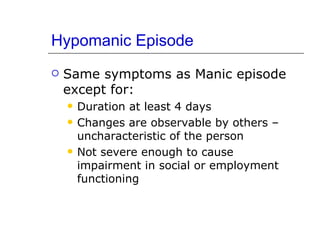
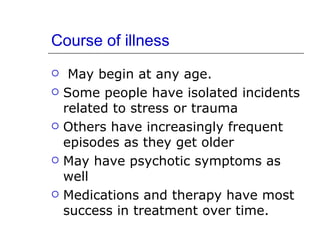
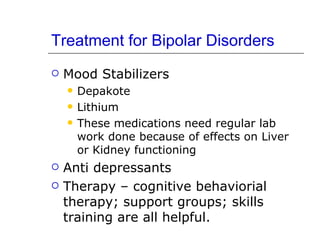
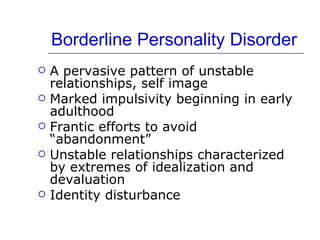
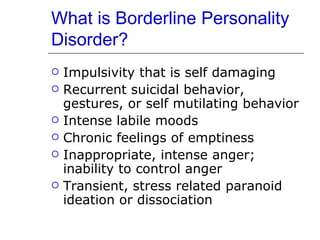
This document provides an overview of several common mental health disorders including schizophrenia, major depression, bipolar disorder, and borderline personality disorder. It discusses the causes and symptoms of each disorder as well as treatment approaches. Key points include that the causes of mental illness involve both genetic and environmental factors, schizophrenia affects about 1% of the global population, and treatments focus on medications as well as therapies like cognitive behavioral therapy and skills training. Recovery is possible for people with mental illness through hope, appropriate treatment and supports, and management of ongoing symptoms.