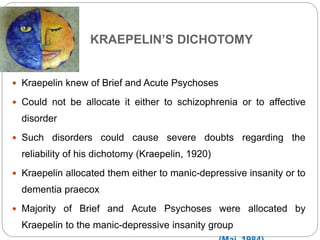
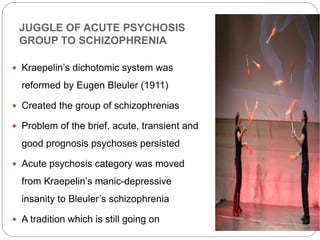
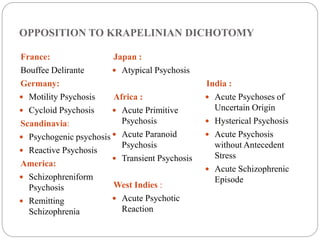
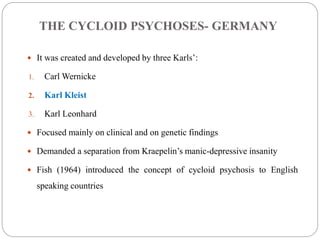
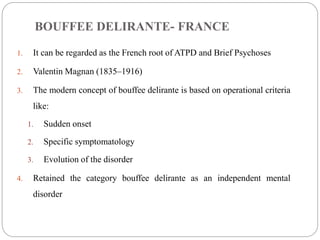
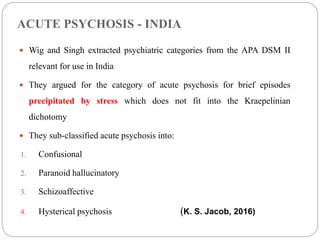
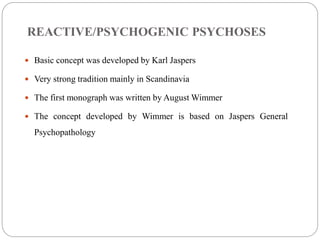
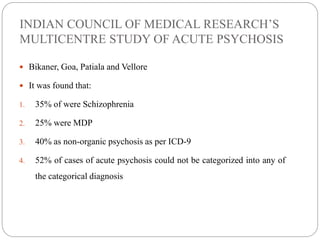
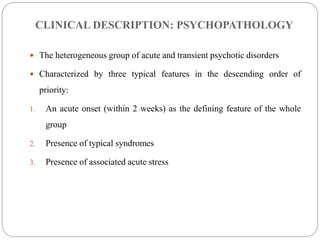
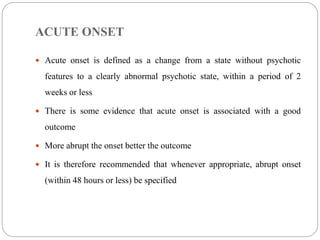
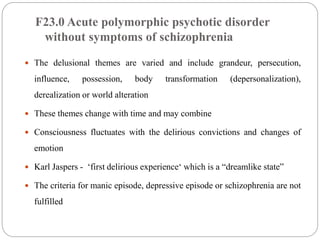
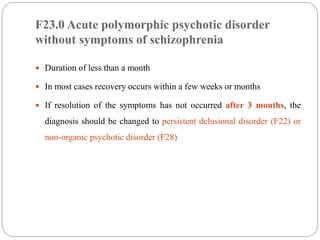
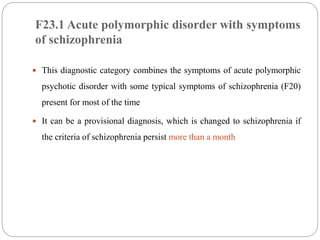
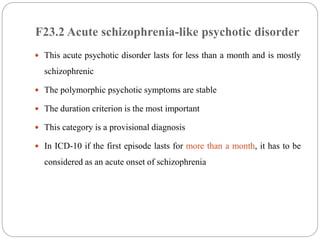
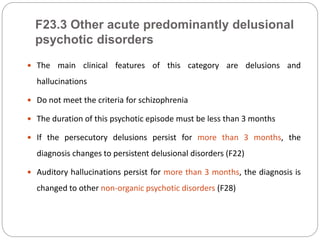
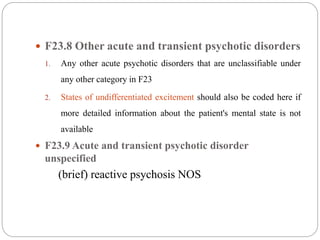
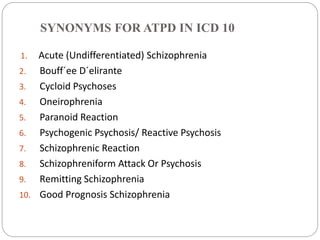
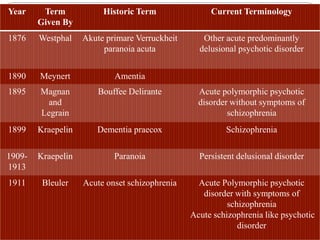
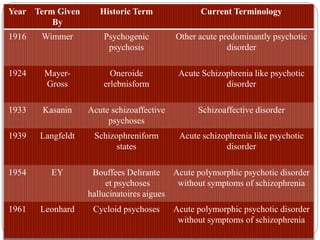
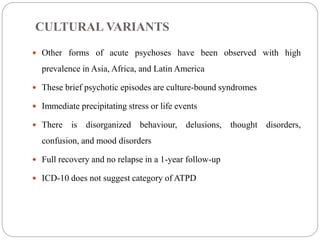
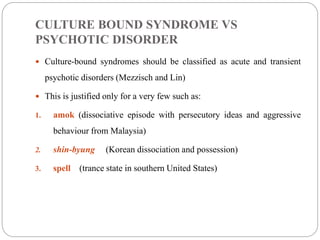
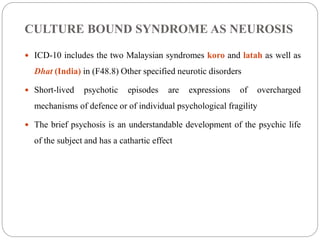
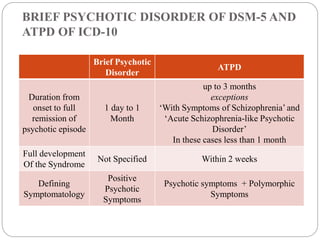
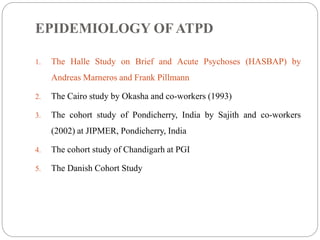
This document provides an overview of Acute and Transient Psychotic Disorder (ATPD). It discusses the history and evolution of ATPD from early descriptions in the late 19th century to its inclusion as a diagnostic category in ICD-10 in 1992. The document outlines the ICD-10 diagnostic criteria for ATPD and reviews several landmark studies that helped establish ATPD as a separate diagnostic category from schizophrenia and affective disorders. It also discusses cultural variants of brief psychotic episodes and debates around classifying certain culture-bound syndromes as ATPD.